 Open Access
Open Access
CASE REPORT
Percutaneous Transcatheter Closure of Congenital Atrial Septal Defect with Scoliosis under Transthoracic Echocardiography Guidance
1 Heart Center and Department of Ultrasound, Women and Children’s Hospital, Qingdao University, Qingdao, 266000, China
2 Qingdao Central Hospital, University of Health and Rehabilitation Sciences, Qingdao, 266000, China
* Corresponding Author: Silin Pan. Email:
# These authors contributed equally to this work
(This article belongs to the Special Issue: Novel Methods and Techniques for the Management of Congenital Heart Disease)
Congenital Heart Disease 2025, 20(2), 195-200. https://doi.org/10.32604/chd.2025.063682
Received 21 January 2025; Accepted 03 April 2025; Issue published 30 April 2025
Abstract
Congenital atrial septal defect (ASD) with severe scoliosis is a rare compound malformation in children. Severe scoliosis should be corrected as soon as possible. The growth rod is suitable for patients with early scoliosis and obvious scoliosis under 10 years old. However, the fluoroscopic radiopaque of titanium alloy plate will inevitably partly make the operative field of interventional occlusion blind. We present a 7-year-old Chinese girl with ASD and scoliosis who underwent spinal correction with a dual-growth rod. In this case, we performed transcatheter closure of ASD solely under the guidance of transthoracic echocardiography. Transthoracic echocardiography (TTE) has been reported as efficacious and safe for assessment and guidance of ASD occlusion. For patients with visual field occlusion under fluoroscopy, the application of TTE is efficacious and safe for assessment and guidance of ASD occlusionKeywords
Supplementary Material
Supplementary Material FileA 7-year-old girl was taken to Women and Children’s Hospital, Qingdao University for a heart murmur. Echocardiography (Echo) showed atrial septal defect (ASD) of 13 mm (Fig. 1) with enlarged right atrium and right ventricle, slightly dilated pulmonary artery (17 mm), and left ventricular ejection fraction (LVEF) of 65%. Due to severe scoliosis, the girl underwent five spinal operations and dual growth rods at Beijing Children’s Hospital. It is indicated by our physical examination that the child had a thoracic deformity with left chest collapse.
Three-dimensional reconstruction of the thorax showed bilateral thoracic asymmetry, the 4th, 5th, and 6th rib fused posteriorly, the 6th, 7th, 9th, and 10th ribs on the left side were obviously widened, and the spine was significantly convex to the left side (Fig. 2). Chest fluoroscopic imaging of the corrective device may generate an influence on the field of vision of interventional occlusion (Fig. 3). Based on our previous experience, we decided to perform ASD closure solely under the guidance of Transthoracic Echocardiography (TTE). The size and location of ASD, the length and hardness of the defect rim, pulmonary hypertension, and blood flow direction of the defect were evaluated from the apical four-chamber view, subcostal sagittal view, and parasternal short-axis view (Philips IE33). The written informed consent was obtained from the parents.
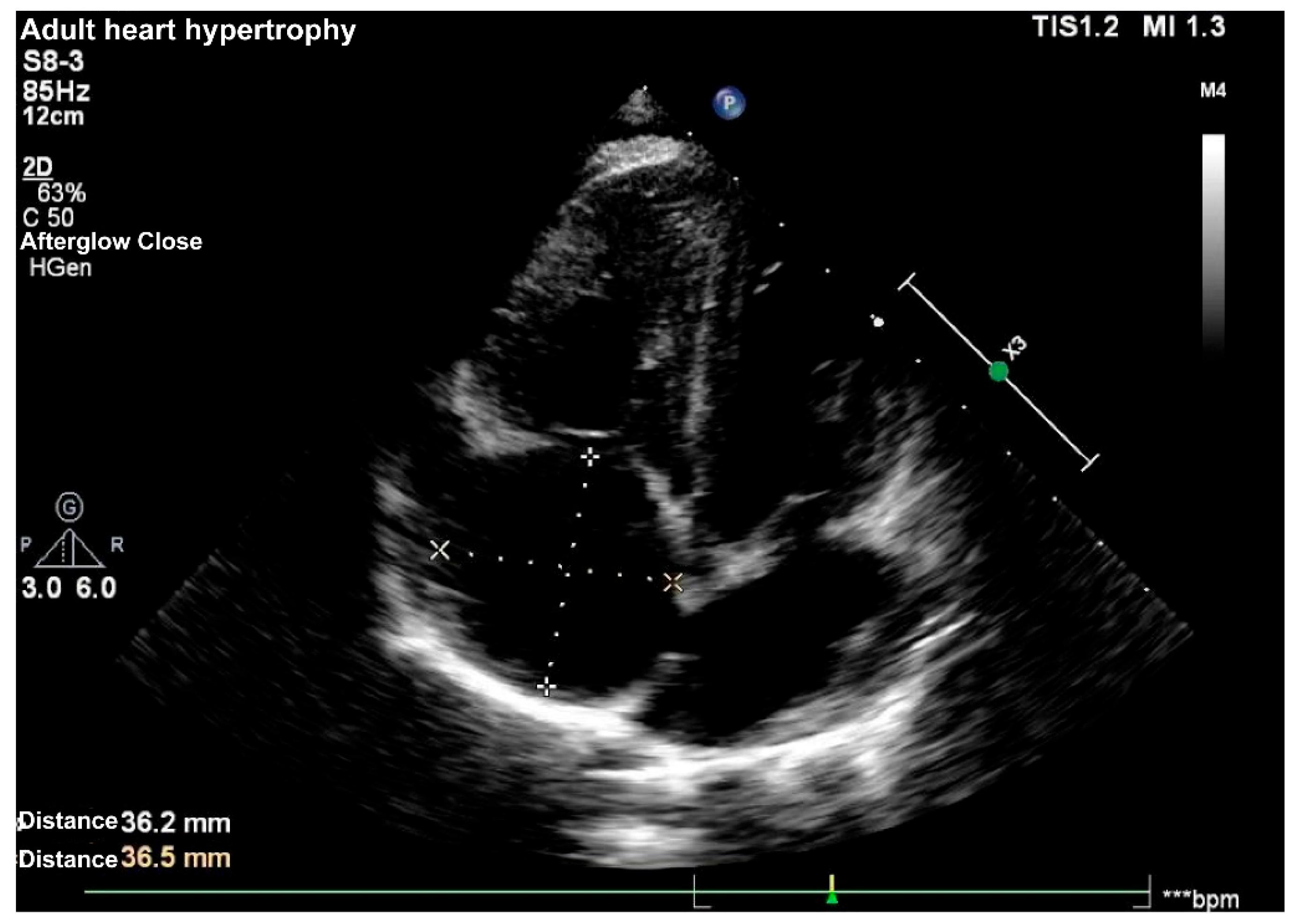
Figure 1: Apical four-chamber view of the heart revealing dilated right atrium and right ventricle and the atrial septum deleted 13 mm.
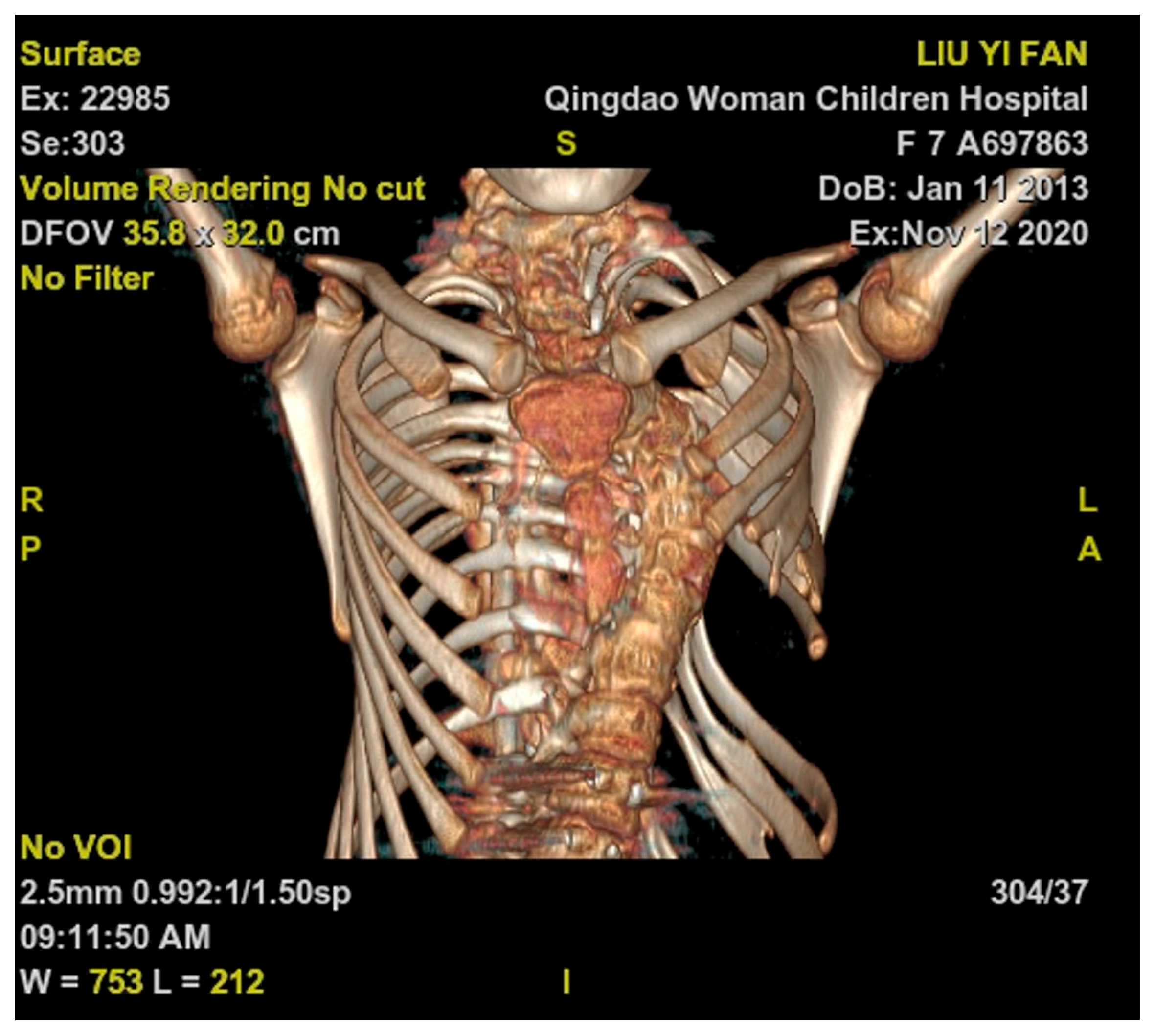
Figure 2: Three-dimensional reconstruction of thoracic bones showed bilateral thoracic asymmetry, the 4th, 5th, and 6th ribs fused posteriorly, and the 6th, 7th, 9th, and 10th ribs on the left side were widened.
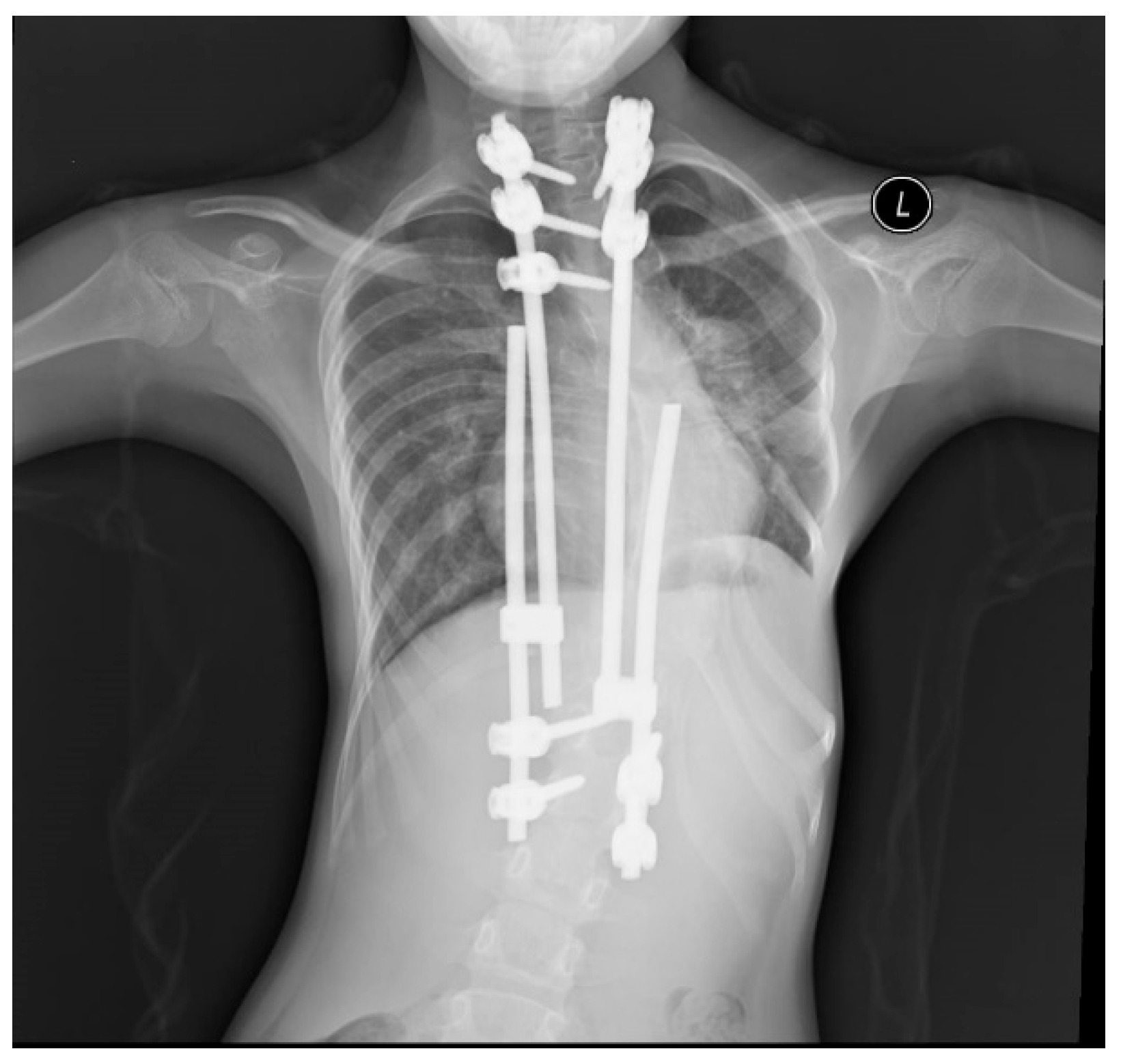
Figure 3: Chest radiograph showed that the spine was corrected by a dual growth rod.
Under general anesthesia, a right femoral vein was punctured. Heparin was administered intravenously, and the activated clotting time was continuously monitored throughout the surgical procedure, maintaining it at over 220 s.
The length was marked on a 6Fr multifunctional catheter to indicate the distance from the puncture site to the right atrium, before being advanced through the inferior vena cava to the right atrium. Under the direction of real-time TTE, adjusting the angle, direction, and depth of the tip of the multifunctional catheter, it entered into the left atrium through the ASD. Feed the stiffened guide wire along the catheter, fix the guide wire in the left lower pulmonary vein, withdraw the catheter, feed the 8Fr delivery sheath along the stiffened guide wire to the left atrium, and withdraw the delivery sheath core and the guide wire. Under the guidance of TTE, the 16 mm occluder was pushed into the sheath. The left and right atrial disks were released in sequence. The shape of the occluder, position, and atrioventricular valve function were assessed by TTE (Fig. 4). Finally, the delivery sheath was removed, and compression bandages were applied. The operation time lasted 30 min. Aspirin was given (3–5 mg/kg, orally) every day for 6 months. The girl recovered and was discharged from the hospital 3 days after the intervention. There were no major cardiovascular-related complications.
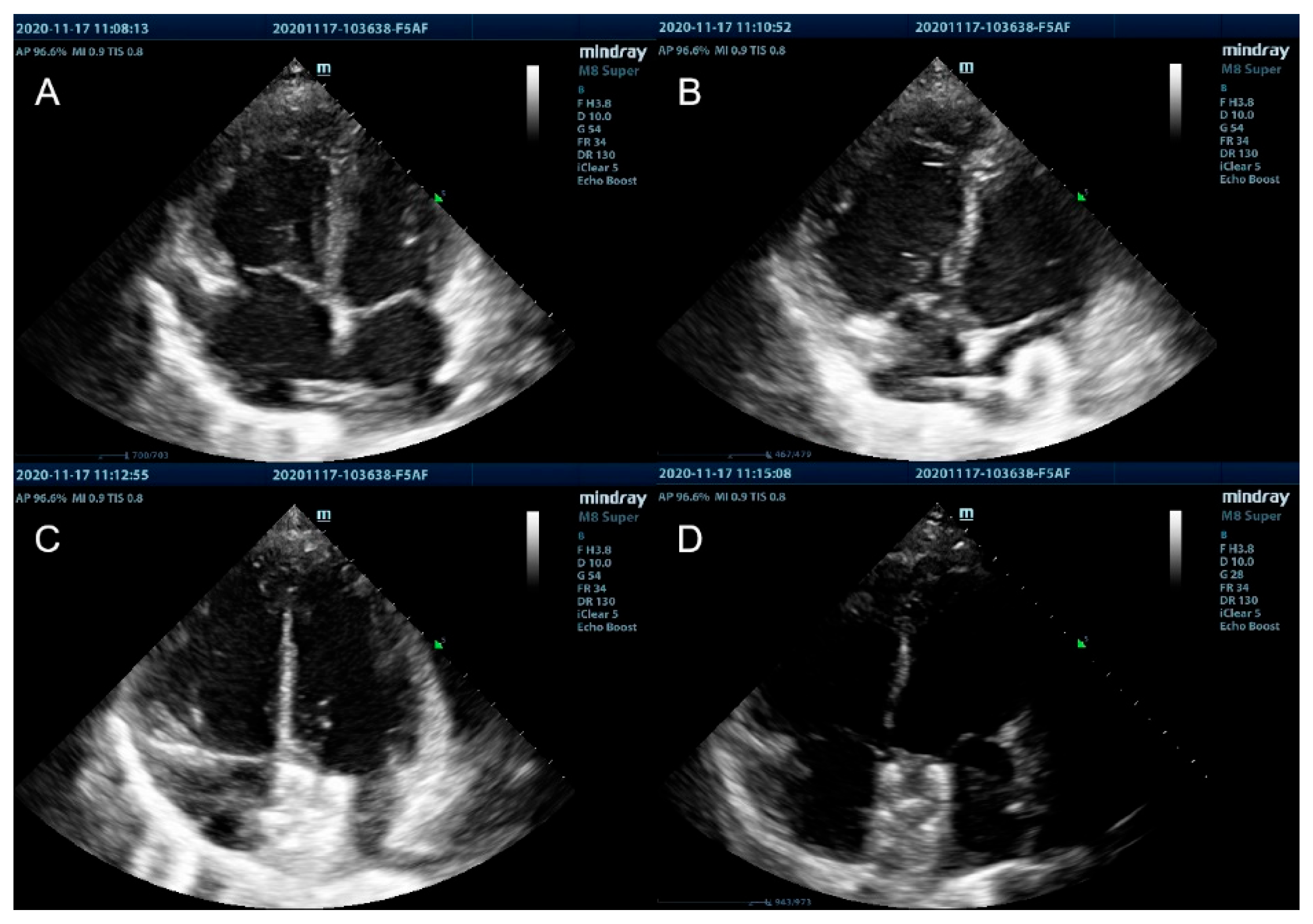
Figure 4: (A) Apical four-chamber view of the heart revealing the multifunctional catheter was advanced through the ASD to the left atrium. (B) Under the guidance of real-time TTE, the left atrial disc of the occluder was opened and pulled back parallel to the atrial septum. (C) Under the guidance of real-time TTE, the right disc was sequentially opened to close the ASD. (D) After checking the occluder’s immobility and the possible presence of a residual shunt, the occluder was released.
The relationship between congenital heart disease (CHD) and congenital scoliosis has been explored for several decades [1]. Children with CHD are more likely to develop spinal and thoracic deformities in the fetal period or thoracic scoliosis after thoracic surgery [2,3,4]. Severe scoliosis with spinal rotation often occurs after surgical treatment of congenital heart disease [5]. Current evidence suggests a 10-fold increase in the prevalence of scoliosis in children with CHD compared with age-matched populations. The surgical treatment of CHD is reported to be associated with a high prevalence of scoliosis [6,7]. We introduce an exceptional instance of transcatheter closure of an ASD, a procedure that was uniquely navigated exclusively through Transthoracic Echocardiography (TTE). This particular case stands out due to the prior spinal corrective surgery of the patient, which involved the insertion of a dual growth rod, rendering X-ray fluoroscopy unsuitable for guiding the transcatheter treatment. Despite this earlier surgical procedure, the ASD closure was subsequently accomplished with remarkable success, solely relying on TTE throughout.
Clinically, Transesophageal Echocardiography (TEE) guided ASD closure has become a development trend in recent years [8]. The Echo presents prominent advantages for ASD intervention compared with fluoroscopy. TEE can visually display the influence of the occluder on the atrioventricular valve, coronary sinus, pulmonary vein, and adjoined tissues, and real-time monitoring of the procedure process, capable of occluder replacement if improperly positioned [9].
However, TEE is an invasive procedure that requires the insertion of an esophageal probe and general anesthesia with tracheal intubation to avoid aspiration, which increases the incidence of complications and costs. TTE provides high-resolution views of ASD itself and the spatial orientations regarding neighboring structures, offering indispensable information that can be substituted with TEE in pediatric patients [10]. However, there is no consensus regarding TTE being applied individually in ASD transcatheter closures. Although it is generally recognized internationally that cases with maldeveloped inferior and posterior borders as well as superior border defects pose certain risks when assessed using TTE, the effectiveness of TTE in cases without these conditions is not significantly different from that of TEE [11]. As confirmed by many experts, TTE can serve as a reliable tool for measuring the diameter of ASD and providing guidance during device closure when operated by skilled hands [12,13].
It is difficult for beginners to guide ASD closure with TTE merely. Regarding each step of the operation, the atrial septum needs to be observed from different perspectives, which requires the operator to be especially familiar with the two-dimensional anatomical spatial structure of the heart [14]. The operation time is relatively long, requiring the surgeon to make psychological preparations before the operation and communicate with the family about the expected operation time. Under routine circumstances, it is usually not easy to locate the tip of the catheter through the apical four-chamber view, parasternal long-axis view, and subxiphoid acoustic window. There are some difficulties in this section without fluoroscopy. Therefore, we have to rotate the catheter to assist its visualization from the Echo. It is required to mark the catheter with a sterile mark pen before insertion to indicate the distance from the puncture point to the apex of the heart. Under the guidance of TTE, the occluder was delivered through the sheath by pushing the cable slowly. The left and right atrial disc of the occluder was released in turns.
Congenital heart disease with scoliosis is a rare compound malformation [15]. For children of a spinal implanted plate with relative intervention contraindications, TTE is possibly a better alternative for the guidance of ASD occlusion. In conclusion, this report describes a successful case of transcatheter ASD closure guided entirely by TTE. It is suggested by this study that in selected pediatric patients with visual field occlusion under fluoroscopy, the application of TTE is efficacious and safe for assessment and guidance of ASD occlusion.
Acknowledgement:
Funding Statement: This research was supported by the National Natural Science Foundation of China (82271725).
Author Contributions: Yaqi Tang, Gang Luo, Huashu Liu, and Hao Wan carried out the studies, participated in collecting data, drafted the manuscript, and helped to draft the manuscript. Hao Wan and Silin Pan operated and participated in its design. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics Approval: The studies involving human participants were reviewed and approved by Women and Children’s Hospital, Qingdao University (QFELL-KY-2022-64). Written informed consent to participate in this study was provided by the participant’s legal guardian. Written informed consent was obtained from the minor(s)’ legal guardian, for the publication of any potentially identifiable images or data included in this article.
Informed Consent: Informed written consent was obtained from the minor(s)’ legal guardian for the publication of this case report.
Conflicts of Interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Materials: The CARE checklist has been provided as a supplementary file online at https://www.techscience.com/doi/10.32604/chd.2025.063682/s1.
Abbreviations
| Atrial Septal Defect | |
| Echocardiography | |
| Left Ventricular Ejection Fraction | |
| Congenital Heart Disease | |
| Transthoracic Echocardiography | |
| Transesophageal echocardiography |
References
1. Cheng JC, Castelein RM, Chu WC, Danielsson AJ, Dobbs MB, Grivas TB, et al. Adolescent idiopathic scoliosis. Nat Rev Dis Primers. 2015;1:15030. doi:10.1038/nrdp.2015.30. [Google Scholar] [CrossRef]
2. Furdock R, Brouillet K, Luhmann SJ. Organ system anomalies associated with congenital scoliosis: a retrospective study of 305 patients. J Pediatr Orthop. 2019;39(3):190–4. doi:10.1097/BPO.0000000000001279. [Google Scholar] [CrossRef]
3. Passias PG, Poorman GW, Jalai CM, Diebo BG, Vira S, Horn SR, et al. Incidence of congenital spinal abnormalities among pediatric patients and their association with scoliosis and systemic anomalies. J Pediatr Orthop. 2019;39(8):608–13. doi:10.1097/BPO.0000000000001066. [Google Scholar] [CrossRef]
4. Homans JF, de Reuver S, Heung T, Silversides CK, Oechslin EN, Houben ML, et al. The role of 22q11.2 deletion syndrome in the relationship between congenital heart disease and scoliosis. Spine J. 2020;20(6):956–63. doi:10.1016/j.spinee.2020.01.006. [Google Scholar] [CrossRef]
5. Kaito T, Shimada M, Ichikawa H, Makino T, Takenaka S, Sakai Y, et al. Prevalence of and predictive factors for scoliosis after surgery for congenital heart disease in the first year of life. JB JS Open Access. 2018;3(1):e0045. doi:10.2106/JBJS.OA.17.00045. [Google Scholar] [CrossRef]
6. Balubaid RN, Aljedani RS, Moglan A, Hennawi YB, Mousa AH, Alosaimi M. Prevalence of spinal deformity development after surgical management of a congenital heart disease among children: a systematic review and meta-analysis. Eur Spine J. 2024;33(5):2088–96. doi:10.1007/s00586-023-08083-8. [Google Scholar] [CrossRef]
7. Przybylski R, Hedequist DJ, Nasr VG, McCann ME, Brustowicz RM, Emans JB, et al. Adverse Perioperative Events in Children with Complex Congenital Heart Disease Undergoing Operative Scoliosis Repair in the Contemporary Era. Pediatr Cardiol. 2019;40(7):1468–75. doi:10.1007/s00246-019-02169-1. [Google Scholar] [CrossRef]
8. Xu W, Li J, Ye J, Yu J, Yu J, Zhang Z. Transesophageal echocardiography and fluoroscopy for percutaneous closure of atrial septal defects: a comparative study. Medicine. 2018;97(43):e12891. doi:10.1097/MD.0000000000012891. [Google Scholar] [CrossRef]
9. Ke Q, Weng G, Xie Q, Bao J, Zheng F, Huang J, et al. Comparison of long-term clinical outcomes and costs between transesophageal echocardiography-guided and X-ray-guided percutaneous atrial septal defect closure in children. Pediatr Cardiol. 2024. doi:10.1007/s00246-024-03539-0. [Google Scholar] [CrossRef]
10. Azhar AS. Safety and efficacy of transthoracic versus transesophageal echocardiography in transcatheter closure of atrial septal defects: reporting a single center experience from Saudi Arabia. Saudi Med J. 2016;37(11):1196–205. doi:10.15537/smj.2016.11.15617. [Google Scholar] [CrossRef]
11. Xie LF, Lin Y, Chen MF, Zhang GC. Complete transthoracic echocardiography for the assessment and guidance of percutaneous atrial septal defect closure in adults without balloon sizing: an Observed Study with a 10-Year Follow-Up. J Cardiovasc Dev Dis. 2023;10(8):321. doi:10.3390/jcdd10080321. [Google Scholar] [CrossRef]
12. Pan XB, Ou-Yang WB, Pang KJ, Zhang FW, Wang SZ, Liu Y, et al. Percutaneous Closure of Atrial Septal Defects Under Transthoracic Echocardiography Guidance Without Fluoroscopy or Intubation in Children. J Intervent Cardiol. 2015;28(4):390–5. doi:10.1111/joic.12214. [Google Scholar] [CrossRef]
13. Chen Q, Cao H, Zhang GC, Chen LW, Lu H, Yu LL. Transcatheter device closure of atrial septal defects guided completely by transthoracic echocardiography: a single cardiac center experience with 152 cases. Anatol J Cardiol. 2018;20(6):330–5. doi:10.14744/AnatolJCardiol.2018.90502. [Google Scholar] [CrossRef]
14. Huang LL, Wu J, Chen M, Jiang CL, Zeng C, Su CX, et al. Transcatheter closure of atrial septal defect with deficient posterior-inferior or inferior vena cava rim under echocardiography only: a feasibility and safety analysis. Cardiol Young. 2022;32(4):589–96. doi:10.1017/S104795112100264X. [Google Scholar] [CrossRef]
15. Yamaguchi K, Uehara M, Oba H, Hatakenaka T, Kuraishi S, Ikegami S, et al. Hemoptysis due to progressive scoliosis associated with congenital heart disease: a case report. BMC Musculoskelet Disord. 2022;23(1):263. doi:10.1186/s12891-022-05225-9. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools