 Open Access
Open Access
MINI REVIEW
Review of techniques and approaches for ectopic reservoir placement in inflatable penile implant
1 Department of Urology, Rambam Health Care Campus, Haifa, 3109601, Israel
2 Sexual Health, Reuth Rehabilitation Hospital, Tel-Aviv, 6772829, Israel
* Corresponding Author: Etan Eigner. Email:
Canadian Journal of Urology 2025, 32(3), 229-235. https://doi.org/10.32604/cju.2025.063332
Received 12 January 2025; Accepted 29 April 2025; Issue published 27 June 2025
Abstract
Inflatable penile prosthesis (IPP) implantation is the gold standard treatment for patients with erectile dysfunction who are refractory to medical therapy. The standard placement of the reservoir in the space of Retzius (SOR) may be contraindicated in patients with prior pelvic or abdominal surgery due to altered anatomy and increased risk of complications. This has led to the development of alternative ectopic reservoir placement techniques. In this narrative review, we summarize the literature on various ectopic reservoir approaches, including low and high submuscular placements, submuscular techniques with counter incisions or transfascial fixation, midline submuscular placement, subcutaneous placement, and lateral retroperitoneal approaches. We describe the surgical methods, outcomes, and complication rates associated with each technique. While most methods demonstrate low complication and revision rates, direct comparisons remain limited due to heterogeneity and lack of prospective data. This review highlights the importance of individualized technique selection based on prior surgical history, body habitus, and surgeon experience. As ectopic placement becomes more widely adopted, familiarity with multiple approaches is essential for prosthetic surgeons.Keywords
Inflatable penile prosthesis (IPP) is considered the gold standard treatment aiming to restore sexual function for motivated patients with erectile dysfunction (ED) who have not achieved satisfactory results with oral medications, penile injections, vacuum devices, or any other modality. With ED becoming increasingly prevalent, the number of penile implants is on the rise.1,2
Routinely, the reservoir of the three-piece IPP is placed in the space of Retzius (SOR). Placement is performed by gaining access via an extra-peritoneal approach through the external inguinal ring and piercing the transversalis fascia.3
Access to the SOR can be compromised or obliterated as a result of previous abdominal/pelvic surgery such as radical prostatectomy, radical cystectomy, inguinal hernia repair, or kidney transplantation. Complications of reservoir placement in the SOR include bladder, vascular, or bowel injuries, reservoir herniation or migration, and dislocation.4–6
This challenge has led to the development of a myriad of techniques, with the common strategy being the use of an ectopic reservoir location.
The first description of an ectopic reservoir placement was in 2001 by Wilson et al.7 The reservoir was placed superior to the transversalis fascia and beneath the abdominal musculature. This method did not gain traction due to the resultant groin location of the reservoir tending to be palpable and occasionally herniating to the scrotum.8
Since then, many more techniques have been proposed and practiced. In this article, we review the locations and approaches described for ectopic IPP reservoirs. These include intra-abdominal, high sub-muscular, subcutaneous, midline sub-muscular, and within the retro-peritoneum.
A comprehensive search strategy was employed to identify relevant studies for inclusion in this review article. The search was conducted in electronic databases including PubMed/MEDLINE, Embase, Cochrane Library, and Google Scholar. Search terms were carefully selected to capture a comprehensive range of relevant articles. Medical Subject Headings (MeSH) terms and keywords were utilized, incorporating variations related to penile implants. The literature search encompassed articles published between 1990 and 2024.
Studies were included in the review if they met the following criteria: 1. Reported a novel technique/location or included a large cohort on an established technique. 2. Published in peer-reviewed journals. 3. Written in English.
In 2011, Perito et al. introduced enhancements to Wilson’s technique.9 They offered two reservoir placements differing from each other based on their relationship to the transversalis fascia. Their study described a cephalad reservoir placement either posteriorly (PTF) or anteriorly (ATF) to the transversalis fascia through a penoscrotal incision. In patients who were at risk for complications with the standard SOR placement, they recommended the ATF approach. In this method, a long nasal speculum passes through the external ring, and then forcibly advances the cephalad reservoir without perforation of the transversalis fascia. Thus, the superior wall of the inguinal canal is perforated. The space is developed between the transversalis fascia and the overlying rectus abdominis muscle.
Stember et al.10 reported their experience with this technique, they followed 447 patients who underwent reservoir placement in the ATF method. Among this cohort, only two (0.4%) patients were elected for revision surgery due to bothersome palpation of the reservoir. Fifteen patients (3%) felt the reservoir in the early postoperative period but later reported satisfaction. Six (1.3%) patients suffered reservoir herniation into the inguinal canal necessitating additional surgery.
Low submuscular with transfascial fixation
To address the goal of achieving effective reservoir concealment and minimizing reservoir herniation rates, the Low submuscular with transracial fixation technique was developed by Khoei et al.11 In this technique, the reservoir is placed in a low submuscular position anterior to the transversalis fascia and posterior to the rectus muscle. The fascia is used to anchor the reservoir and tubing in place.
The same authors reported their experience with 31 patients.11 In a follow-up of 15 to 34 months, 8 patients (26%) were able to palpate the reservoir, and 4 patients (15.4%) were able to see the reservoir. However, overall satisfaction with reservoir concealment was 4.5 (out of 5). One patient (3.8%) suffered pain from the reservoir with minimal severity. They reported that there were no surgical revisions required or complications.
The ``high sub-muscular” approach is similar to the aforementioned techniques but with an even more cephalad location.12 In this technique, A potential space between the transversalis fascia and rectus abdominis muscle is created through blunt dissection. A forester clamp is used to further separate these layers and then for grasping and delivering the reservoir to its final location.
Morey et al.12 reported their experience with this technique. They implanted 120 submuscular balloons/reservoirs through a penoscrotal approach in 107 patients who underwent either IPP, artificial urinary sphincter, or both. The majority of patients were unable to palpate their reservoir/balloon. Two patients (1.6%) presented with a palpable balloon/reservoir. One had a reservoir herniation and the other was placed into a subcutaneous location. No major complications were reported.
Pagliara et al.13 described their experience with 399 patients who underwent a high submuscular approach reservoir implantation for either IPP or artificial urethral sphincter (AUS) implantation (255 IPP, 144 AUS) With a mean follow-up of 25.6 months, repositioning was required in 8 cases (2%)-half due to pain and half due to herniation. The authors did not note any difference in complication rates between these patients and patients who underwent a standard SOR placement in their institute.
The high submuscular technique is essentially a blind placement of the reservoir. A previous cadaveric study has already called into question the accuracy of the final location of the reservoir, with only 35% of the reservoirs placed in the intended high sub-muscular position.14
The use of an inguinal counter incision (CI) for the sub-muscular placement of the reservoir offers a few theoretical advantages: decreased risk of vascular or organ damage during placement and decreased herniation rates due to the avoidance of external ring manipulation. These advantages come at the cost of increased risk for infection and impaired cosmetic outcomes.15
Grimberg et al.15 compared the outcomes of patients undergoing counter-incision reservoir placement and those with non-counter-incision reservoir placement. The CI group, comprising 51 patients and accounting for 9.6% of the cohort, was demographically comparable to the non-CI group. Despite a higher level of complexity, as reflected by increased rates of removal and replacement cases, the CI group exhibited similar complication rates to the non-CI patients.
In 2010, Hartman et al. first published about the utilization of a counter incision.16 They described a lateral retroperitoneal (LR) placement. In this method, the counter incision is performed 2 cm medially and inferiorly from the anterior superior iliac spine. Dissection is performed until the external oblique fascia, an incision is made, and the external and internal oblique muscles are spread traumatically. Next, the transversalis fascia is bluntly dissected and the retroperitoneal space is developed with the use of a finger.
The outcomes of 266 patients who underwent this procedure with a median follow-up of 20.1 months were published in 2021. There was one (0.3%) instance of intraoperative injury to the colon. Overall, only 6 (2.3%) of patients suffered complications related to the reservoir, such as bulge, pain, or reservoir leaks.
During follow-up, no cases of bladder, bowel, or vascular injury were reported. Compared to standard SOR replacement performed at the same institute, there were no significant differences in complications or revision rates.17
Midline sub-muscular reservoir (MSMR)
The midline sub-muscular rectus reservoir (MSMR) is a novel technique that obviates the need to enter the inguinal ring. In this technique, after pubic tubercle identification, dissection is carried cephalad to the level of the rectus fascia. The fascia is entered lateral to the linea alba, and the rectus sheath is bluntly separated from the posterior sheath of the rectus, creating a submuscular space between the rectus muscle and the posterior sheath.18
This method presents a few advantages. Reservoir placement is done under direct visualization, thus minimizing the potential pitfalls of a blind placement. The method utilizes the peno-scrotal incision without the need for a counter incision. In thin patients who may require submuscular reservoir placement, the reservoir is often visible at the level of the skin. With this approach, the reservoir is not visible, regardless of the body habitus. In addition, if the need for removal arises in the future the reservoir would be relatively easily accessible.18
Zisman et al.18 retrospectively studied the data of 461 patients who underwent IPP surgery. The MSMR method was used in 48 cases (11%) and was compared to the standard SOR placement. Despite the MSMR group representing the more difficult cases, no statistical difference was found between the groups. This led the authors to conclude that the MSMR group presented a favorable safety profile with a very low complication rate.
The placement of a reservoir is technically challenging for obese male patients, especially if they have previously undergone pelvic surgery. In this case, a subcutaneous reservoir may be a valid alternative to the classic approach. In this regard, patient selection is crucial, since thin patients will suffer from a palpable and even visible reservoir.19
Garber et al.19 described their experience with 8 patients who were selected to undergo this type of reservoir placement intraoperatively. The method can be performed with a scrotal or infrapubic incision. In the scrotal approach, the reservoir is tunneled medially and the neck of the tunnel is approximated with absorbable sutures. When using the infra pubic incision, Scarpa’s and Camper’s fascia were approximated anterior to the reservoir with 2–3 layers of absorbable sutures.
With the exception of one patient who required explantation due to infection of the penile implant. Patients healed uneventfully without reservoir hernias or palpable or visible reservoirs.
While reservoir placement in the SOR is suitable for most patients and associated with a low risk of complications, a significant subset of patients with prior pelvic surgery may face an increased risk of adverse events. Capoccia et al.20 compared complication rates in patients undergoing reservoir placement in the SOR, distinguishing between those with and without a history of pelvic surgery. Their findings showed a 2.8% complication rate in patients with prior pelvic surgery, compared to just 0.01% in those without. This disparity is largely attributed to anatomical alterations caused by previous surgical interventions.
Although rare, major complications can be severe and include bladder perforation,21 bowel injury22 due to intraperitoneal placement, and vascular injuries, particularly to the external iliac vein or its branches.23
Due to these risks, the need for an alternative reservoir placement arose. In the short history since the first ectopic reservoir was placed, numerous techniques have been described (Figure 1). As a general rule, a technique’s simplicity and reproducibility naturally lead to a wider adoption throughout the surgical community.
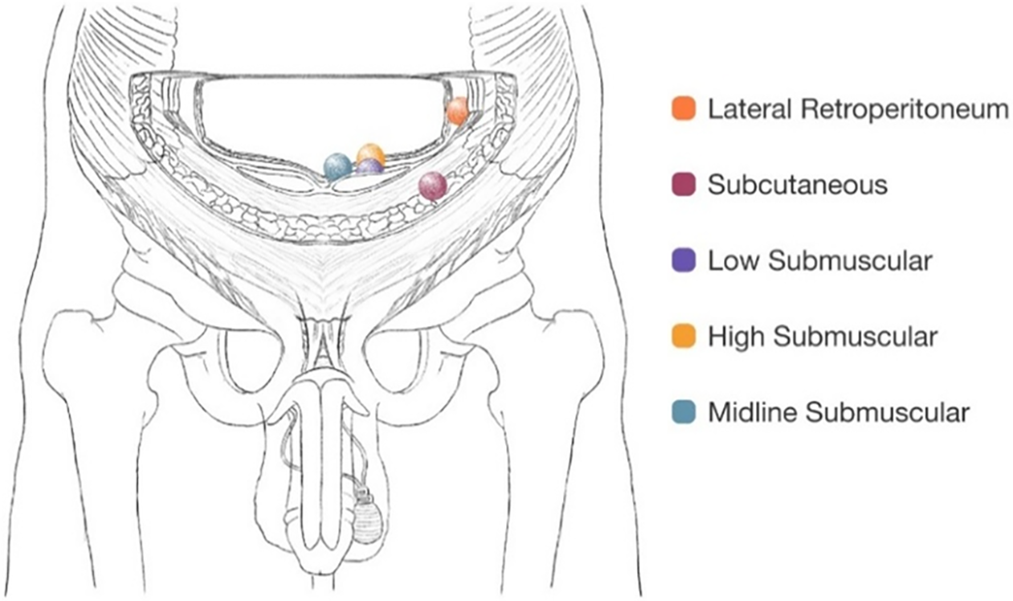
FIGURE 1. Ectopic reservoir locations
The parameters used to assess the feasibility of these techniques are mostly complication and revision rates. The techniques mentioned in this review (Table 1) have all shown promising results, with low complication rates for the traditionally more challenging cases. Drawing conclusions or making recommendations regarding the superiority of one technique over the other is challenging due to the retrospective nature of these studies. Without high-quality randomized and prospective studies comparing the various techniques, it is difficult to ascertain which one may be superior.
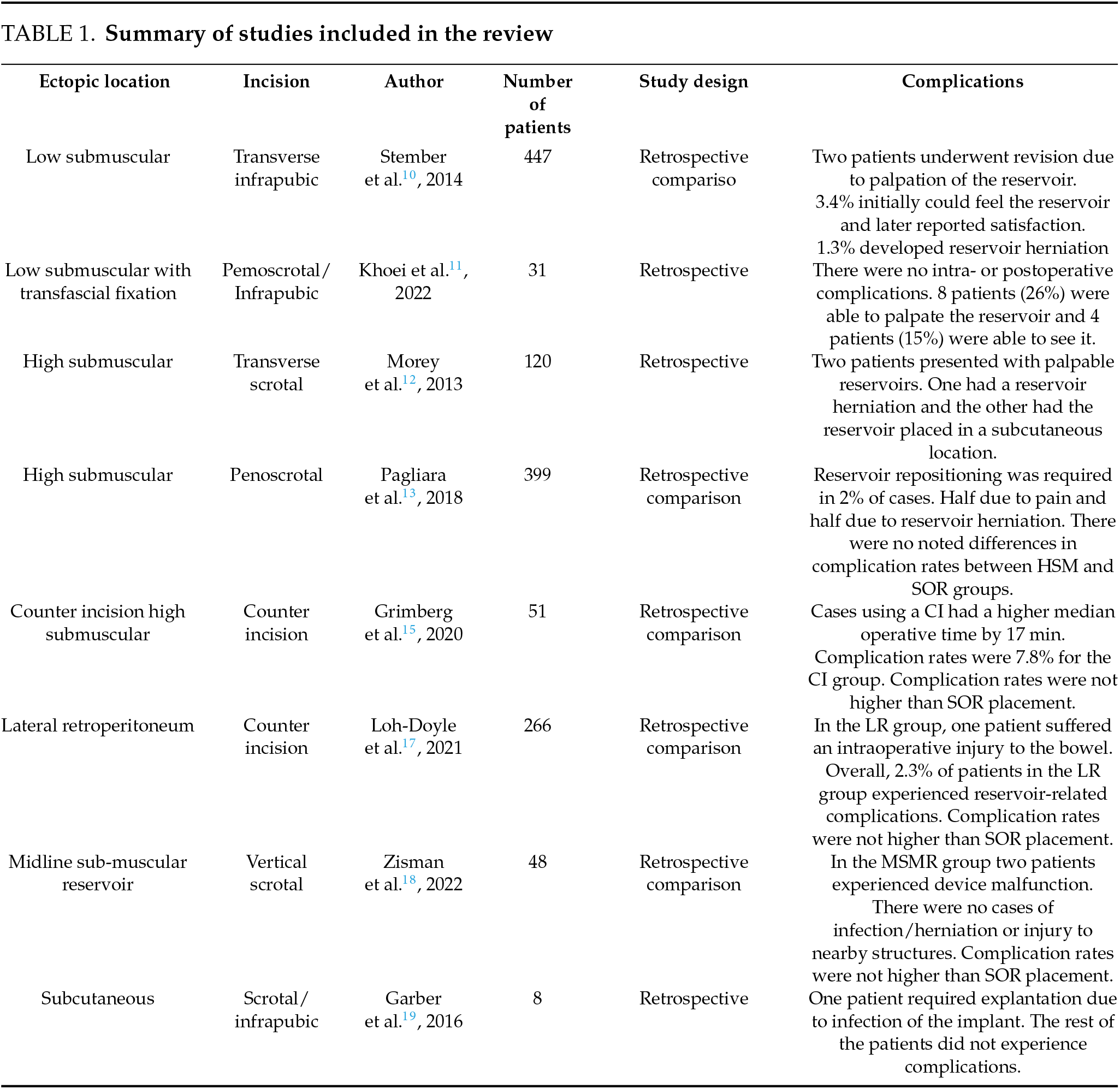
Although direct comparisons between techniques are challenging, it is evident that some methods have been more extensively tested than others. The approach introduced by Perito et al.9 and further evaluated by Stember et al.10 demonstrated reliable outcomes in a cohort of 447 patients, with a remarkably low revision rate of 0.4%. Similarly, the high submuscular technique is supported by substantial evidence, including 120 cases from Morey et al.12 and 399 cases from Pagliara et al.13, both reporting low complication rates (2%) and minimal issues with reservoir palpation or herniation. The lateral retroperitoneal technique, initially described by Hartman et al.16 and later expanded upon by Loh-Doyle et al.17, achieved favorable outcomes with a 2.3% complication rate related to the reservoir. However, this series notably included a case of bowel injury, a complication not reported in other studies.
Hernández et al.23 aimed to better characterize the complications associated with ectopic reservoir placement. In a multi-institutional study spanning five years, they reported their experience with 612 ectopic placements. Of these, 12 cases (2%) required revision due to reservoir-related complications. The most common issue was reservoir leakage, occurring in five cases. Other complications included abdominal pain, tubing torsion, and one incidentally discovered intraperitoneal placement on unrelated imaging.
Due to the proximity of ectopic reservoirs to the abdominal musculature, there was initial concern about an increased risk of herniation. However, reservoir herniation, specifically migration through the inguinal canal remains a rare complication. Karpman et al.24 prospectively studied 759 patients who underwent either SOR or ectopic reservoir placement and found no statistically significant difference in complication rates between the groups, with two cases of herniation reported in each.
Key patient-centered outcomes in ectopic reservoir placement include reservoir palpability and overall patient satisfaction. Modern reservoirs, such as the Coloplast Cloverleaf and American Medical Systems’ Conceal, are designed with a flat configuration to reduce palpability when placed ectopically. Patient satisfaction studies have shown that 94% of patients with high submuscular placement report none or minimal palpability.25 Similarly, Stember et al.10 found that only 2 out of 447 cases required revision due to bothersome palpation.
Currently, the “It Matters” study26 is prospectively assessing patient satisfaction with reservoir placement. Preliminary findings from 34 respondents, including 16 with ectopic placement, indicate that 66.7% (8/12) of patients with ectopic reservoirs reported feeling comfortable or very comfortable, compared to 54.5% (12/22) in the SOR group. However, there were no statistically significant differences in overall satisfaction with reservoir location or physical comfort between the two groups (p = 0.134 and p = 0.623, respectively).
Ectopic reservoir placement has gained widespread acceptance in the prosthetic urology community, with 97% of high-volume, experienced surgeons emphasizing the importance of incorporating ectopic reservoir placement techniques into physician training courses.27 While the indications for the placement of an ectopic reservoir are clear, the approach and location of an ectopic IPP are not standardized. Among the factors that should be taken into account are the patient’s surgical history, body habitus, and individual anatomy. It is also important to consider the surgeon’s experience, familiarity, and preferences with a particular technique when making a decision.
Reconstructive urologists should recognize patients with abnormal pelvic anatomy and be familiar with modern approaches to ectopic IPP placement while tailoring the procedure to suit the individual patient’s needs.
Acknowledgement
The authors would like to express their gratitude to all the researchers, authors and reviewers whose work has contributed to the body of knowledge in the field, upon which this review article is based.
Funding Statement
No financial assistance was received in support of this study.
Author Contributions
Etan Eigner: conducted the initial literature search, identified relevant articles, synthesized the findings, contributed to the conceptualization and design of the review article and drafted the manuscript. Valentin Shabataev: contributed to the interpretation of findings, provided critical feedback on the manuscript, and assisted in finalizing the structure and organization of the review article. Yacov Reisman: contributed to the interpretation of findings, provided critical feedback on the manuscript, and assisted in finalizing the structure and organization of the review article. Ariel Zisman: contributed to the conceptualization and design of the review article, supervised the review process, provided guidance on the overall direction of the manuscript, contributed to the final editing and approval of the manuscript. Nicola Fazza: contributed to the conceptualization and design of the review article and played a role in drafting the manuscript. Ameer Nsair: contributed to the conceptualization and design of the review article and played a role in drafting the manuscript. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials
The data analyzed in this review article are derived from publicly available sources, primarily peer-reviewed journal articles. All sources cited in this review are accessible through standard academic databases and repositories.
Ethics Approval
This review article did not involve primary research data or experiments involving human subjects or animals. Therefore, ethical approval was not required for the conduct of this review.
Conflicts of Interest
The authors declare no conflicts of interest to report regarding the present study.
List of Abbreviations
| ED | Erectile dysfunction |
| IPP | Inflatable penile prosthesis |
| SOR | Space of Retzius |
| MeSH | Medical Subject Headings |
| PTF | Posterior to the transversalis fascia |
| ATF | Anterior to the transversalis fascia |
| AUS | Artificial uretheral sphincter |
| CI | Counter incision |
| MSMR | Midline sub-muscular rectus reservoir |
| LR | Lateral retroperitoneal |
References
1. Baas W, O’Connor B, Welliver C et al. Worldwide trends in penile implantation surgery: data from over 63, 000 implants. Transl Androl Urol 2020;9(1):31–37. doi:10.21037/tau.2019.09.26. [Google Scholar] [PubMed] [CrossRef]
2. Ayta IA, McKinlay JB, Krane RJ. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int 1999;84(1):50–56. doi:10.1046/j.1464-410x.1999.00142.x. [Google Scholar] [PubMed] [CrossRef]
3. Henry G, Hsiao W, Karpman E et al. A guide for inflatable penile prosthesis reservoir placement: pertinent anatomical measurements of the retropubic space. J Sex Med 2014;11(1):273–278. doi:10.1111/jsm.12361. [Google Scholar] [PubMed] [CrossRef]
4. Levine LA, Hoeh MP. Review of penile prosthetic reservoir: complications and presentation of a modified reservoir placement technique. J Sex Med 2012;9(11):2759–2769. doi:10.1111/j.1743-6109.2012.02807.x. [Google Scholar] [PubMed] [CrossRef]
5. Scherzer ND, Dick B, Gabrielson AT, Alzweri LM, Hellstrom WJG. Penile prosthesis complications: planning, prevention, and decision making. Sex Med Rev 2019;7(2):349–359. doi:10.1016/j.sxmr.2018.04.002. [Google Scholar] [PubMed] [CrossRef]
6. Garber BB, Morris A. Intravesical penile implant reservoir: case report, literature review, and strategies for prevention. Int J Impot Res 2013;25(2):41–44. doi:10.1038/ijir.2012.31. [Google Scholar] [PubMed] [CrossRef]
7. Wilson SK, Henry GD, Delk JRJr, Cleves MA. The mentor Alpha 1 penile prosthesis with reservoir lock-out valve: effective prevention of auto-inflation with improved capability for ectopic reservoir placement. J Urol 2002;168(4 Pt 1):1475–1478. doi:10.1016/S0022-5347(05)64477-1. [Google Scholar] [PubMed] [CrossRef]
8. Wilson SK. Ectopic reservoir placement. In: Smith AR, editor. Pearls Perils and Pitfalls of Prosthetic Urology. Textbook of Prosthetic Urology. USA: Calvert Mcbride Printing, 2008. [Google Scholar]
9. Perito PE, Wilson SK. Traditional (retroperitoneal) and abdominal wall (ectopic) reservoir placement. J Sex Med 2011;8(3):656–659. doi:10.1111/j.1743-6109.2011.02202.x. [Google Scholar] [PubMed] [CrossRef]
10. Stember DS, Garber BB, Perito PE. Outcomes of abdominal wall reservoir placement in inflatable penile prosthesis implantation: a safe and efficacious alternative to the space of Retzius. J Sex Med 2014;11(2):605–612. doi:10.1111/jsm.12408. [Google Scholar] [PubMed] [CrossRef]
11. Khoei A, Racik N, Bansal U, Flores F, Khera M. The low submuscular reservoir placement with transfascial fixation for inflatable penile prostheses. J Sex Med 2022;19(8):1309–1312. doi:10.1016/j.jsxm.2022.05.143. [Google Scholar] [PubMed] [CrossRef]
12. Morey AF, Cefalu CA, Hudak SJ. High submuscular placement of urologic prosthetic balloons and reservoirs via transscrotal approach. J Sex Med 2013;10(2):603–610. doi:10.1111/jsm.12000. [Google Scholar] [PubMed] [CrossRef]
13. Pagliara TJ, Viers BR, Scott J, Morey AF. Extended experience with high submuscular placement of urological prosthetic balloons and reservoirs: refined technique for optimal outcomes. Urol Pract 2018;5(4):293–298. doi:10.1016/j.urpr.2017.06.006. [Google Scholar] [PubMed] [CrossRef]
14. Ziegelmann MJ, Viers BR, Lomas DJ, Westerman ME, Trost LW. Ectopic penile prosthesis reservoir placement: an anatomic cadaver model of the high submuscular technique. J Sex Med 2016;13(9):1425–1431. doi:10.1016/j.jsxm.2016.06.012. [Google Scholar] [PubMed] [CrossRef]
15. Grimberg D, Wang S, Carlos E, Nosé B, Harper S, Lentz AC. Counter incision is a safe and effective method for alternative reservoir placement during inflatable penile prosthesis surgery. Transl Androl Urol 2020;9(6):2688–2696. doi:10.21037/tau-20-923. [Google Scholar] [CrossRef]
16. Hartman RJJr, Helfand BT, McVary KT. Outcomes of lateral retroperitoneal reservoir placement of three-piece penile prosthesis in patients following radical prostatectomy. Int J Impot Res 2010;22(4):279–283. doi:10.1038/ijir.2010.16. [Google Scholar] [PubMed] [CrossRef]
17. Loh-Doyle JC, Lin JS, Doumanian LR, Patil MB, Boyd SD. Outcomes of alternative reservoir placement in the lateral retroperitoneum during inflatable penile prosthesis placement. Urology 2021;152:35–41. doi:10.1016/j.urology.2021.02.021. [Google Scholar] [PubMed] [CrossRef]
18. Zisman A, Razdan S, Siegal A et al. Midline submuscular penile prosthesis reservoir placement for patients with bilateral inaccessible inguinal rings: technique and outcomes. Ther Adv Urol 2022;14:17562872221139109. doi:10.1177/17562872221139109. [Google Scholar] [PubMed] [CrossRef]
19. Garber BB, Bickell M. Subcutaneous placement of inflatable penile prosthesis reservoirs. Urology 2016;88:93–96. doi:10.1016/j.urology.2015.10.027. [Google Scholar] [PubMed] [CrossRef]
20. Capoccia EM, Phelps JN, Levine LA. Modified inflatable penile prosthesis reservoir placement into space of retzius: comparing outcomes in men with or without prior pelvic surgery. J Sex Med 2017;14(7):968–973. doi:10.1016/j.jsxm.2017.05.002. [Google Scholar] [PubMed] [CrossRef]
21. Furlow WL, Goldwasser B. Salvage of the eroded inflatable penile prosthesis: a new concept. J Urol 1987;138(2):312–314. doi:10.1016/s0022-5347(17)43131-4. [Google Scholar] [PubMed] [CrossRef]
22. Sadeghi-Nejad H, Munarriz R, Shah N. Intra-abdominal reservoir placement during penile prosthesis surgery in post-robotically assisted laparoscopic radical prostatectomy patients: a case report and practical considerations. J Sex Med 2011;8(5):1547–1550. doi:10.1111/j.1743-6109.2011.02229.x. [Google Scholar] [PubMed] [CrossRef]
23. Hernández JC, Trost L, Köhler T et al. Emerging complications following alternative reservoir placement during inflatable penile prosthesis placement: a 5-year multi-institutional experience. J Urol 2019;201(3):581–586. doi:10.1016/j.juro.2018.10.013. [Google Scholar] [PubMed] [CrossRef]
24. Karpman E, Brant WO, Kansas B et al. Reservoir alternate surgical implantation technique: preliminary outcomes of initial PROPPER study of low profile or spherical reservoir implantation in submuscular location or traditional prevesical space. J Urol 2015;193(1):239–244. doi:10.1016/j.juro.2014.07.082. [Google Scholar] [PubMed] [CrossRef]
25. Chung PH, Morey AF, Tausch TJ, Simhan J, Scott JF. High submuscular placement of urologic prosthetic balloons and reservoirs: 2-year experience and patient-reported outcomes. Urology 2014;84(6):1535–1540. doi:10.1016/j.urology.2014.08.029. [Google Scholar] [PubMed] [CrossRef]
26. Khera M, Carrion R, Tadros N et al. (321) comparing preliminary demographics and patient satisfaction by location of 3-piece ipp reservoir: it matters. J Sex Med 2024;21(Supplement_7):qdae167.311. doi:10.1093/jsxmed/qdae167.311. [Google Scholar] [CrossRef]
27. Karpman E, Sadeghi-Nejad H, Henry G, Khera M, Morey AF. Current opinions on alternative reservoir placement for inflatable penile prosthesis among members of the Sexual Medicine Society of North America. J Sex Med 2013;10(8):2115–2120. doi:10.1111/jsm.12203. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools