 Open Access
Open Access
ARTICLE
The cost burden of radiation cystitis presentations and investigations
Department of Urology, University Hospital Galway, Galway, H91 YR71, Ireland
* Corresponding Author: Brian Gilmartin. Email:
Canadian Journal of Urology 2025, 32(4), 293-298. https://doi.org/10.32604/cju.2025.065805
Received 21 March 2025; Accepted 25 June 2025; Issue published 29 August 2025
Abstract
Background: Radiation cystitis is a well-known complication resulting from radiotherapy for pelvic malignancies. It remains a challenging condition to treat and is associated with significant morbidity for patients. We aimed to establish the economic cost burden of presentations and investigations associated with radiation cystitis over a two-year period to a tertiary referral hospital in Ireland. Materials and Methods: A retrospective review of patient charts was performed for radiation cystitis-related presentations and investigations over 24 months. Costs were estimated in consultation with the hospital finance department and using Health Service Executive data on diagnostic-related groups and average inpatient bed day costs. Results: A total of 56 individual patients were identified over 2 years. 91% male, 9% female. The mean age was 72 years. Twenty-three patients (41%) required inpatient care. Radiation cystitis accounted for 621 inpatient bed days. Median length of stay was 7.5 days. The inpatient care cost was approximately €545,238 (801,908 Canadian dollars (CA$)) over 2 years. Conclusion: Radiation cystitis accounts for a significant amount of inpatient bed days. A conservative estimate of the overall cost burden for inpatient care and outpatient investigations exceeds €280,000 (CA$411,810) per year.Keywords
Radiotherapy (RT) is an accepted treatment modality for a wide range of pelvic malignancies. The main adverse side effects are related to microvasculature damage to organs, with one-third of patients reporting acute symptoms of proctitis or cystitis during treatment.1 In the majority of patients these symptoms improve after completion of treatment; however, with improving disease survival the late side effects of radiotherapy are becoming apparent. Radiation Cystitis (RC) is a term used to describe the side effects of inflammation and subsequent destruction to the normal anatomy of the urinary bladder at the cellular level after the use of radiotherapy.2 RC is a well-recognized complication of pelvic radiotherapy with a reported incidence of 23–80%, with a reported mean duration to symptom onset of 31.8 months post-treatment.2
RC may present as a constellation of symptoms and represents a chronic and complex management challenge. Urinary symptoms include dysuria, frequency, urgency, and haematuria.2,3 The reported incidence of severe hemorrhagic cystitis ranges from 5% to 8% in patients with RC and the onset of haematuria has been reported up to fourteen years post radiotherapy.2,4 The risk of developing haematuria increases with time, with a reported risk of 5.8% at five years and 9.6% at twenty years.5
The management of RC depends on the severity of symptoms with a spectrum of treatment options including oral medications, bladder irrigation, intravesical instillations, hyperbaric oxygen therapy, or surgical intervention.3,6,7 Complications associated with pelvic RT may account for up to 7% of emergent urological admissions, with RC comprising more than half of these.6,8 Although rare, patients with RC may require frequent hospitalisations, investigations, and procedures with a potential economic burden on the healthcare system.
We aimed to establish the economic cost burden associated with radiation cystitis over two years to a tertiary referral center.
Ethical approval was granted by the Clinical Research Ethics Committee of University Hospital Galway (Ref: C.A. 2864). This retrospective study was exempt from informed consent requirements as all data were anonymized. A retrospective review was conducted to identify patients presenting with radiation cystitis (RC) to a tertiary referral hospital over 24 months. Using diagnostic Hospital In-Patient Enquiry (HIPE) coding terms, we identified all presentations to our center with ‘haematuria’ and ‘radiation cystitis’ during the study period. These cases were subsequently reviewed to exclude patients presenting for reasons other than RC.
Patients meeting the inclusion criteria were identified, and each electronic patient record was reviewed to collect data. The collected data included: patient demographics, number of admissions, length of stay, indication for previous radiotherapy, inpatient and outpatient investigations, and treatments. Data were compiled and analyzed using Microsoft Excel, and descriptive statistical analysis was performed.
Using these data, we estimated the financial burden on our institution. Costs were calculated in consultation with the hospital finance department and by utilizing publicly available Health Service Executive (HSE) data on diagnostic-related groups and average inpatient bed-day costs.9 Individual patient costs were aggregated to provide a total combined cost estimate.
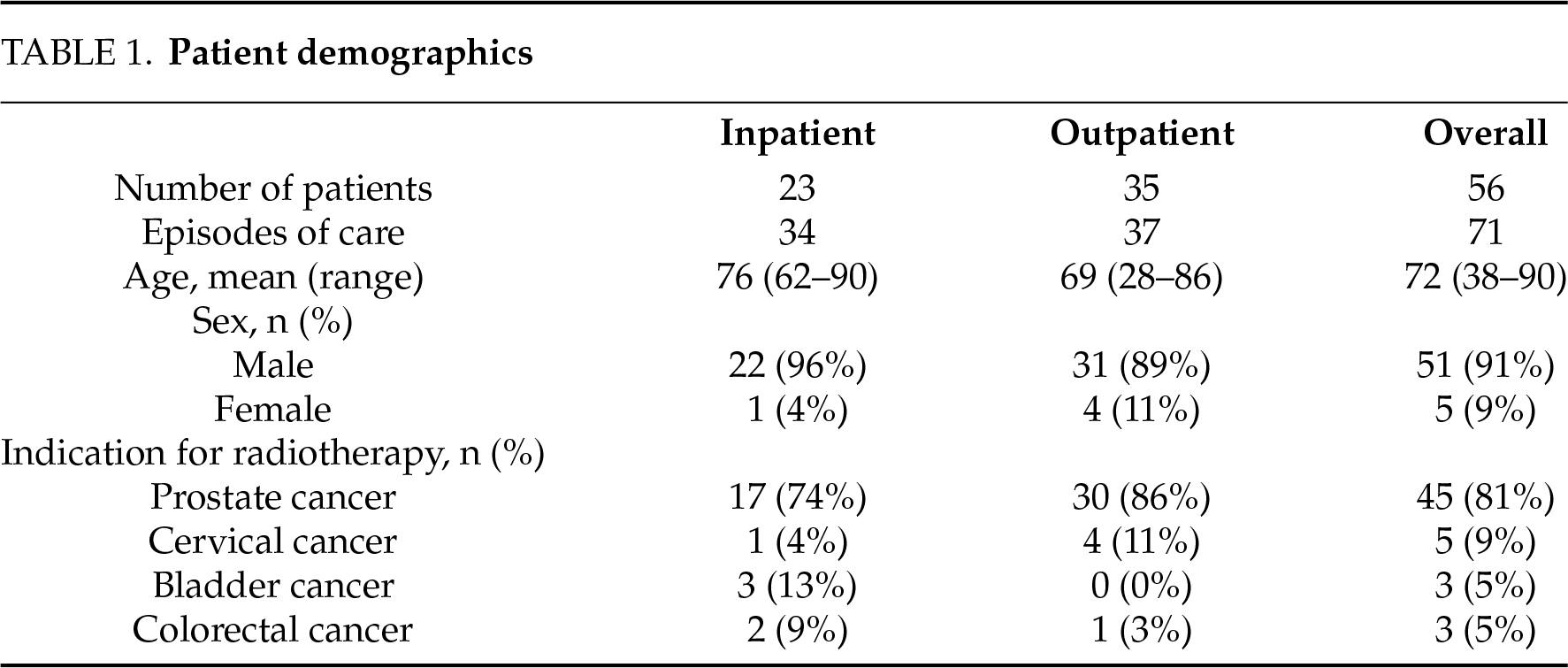
Patient characteristics
A total of 56 individual patients were identified over 2 years with 71 episodes of care. Ninety-one percent (n = 51) of patients were male and 9% (n = 5) were female. The mean age was 72 years (range 38–90). The most common indication for radiotherapy was prostate cancer (n = 45, 81%), followed by cervical cancer (n = 5, 9%), bladder cancer (n = 3, 5%) and colorectal cancer (n = 3, 5%). See Table 1.
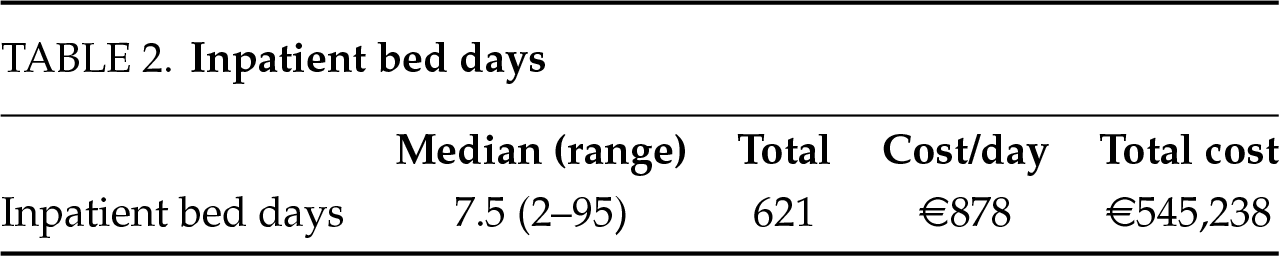
Inpatient admissions
Inpatient care was required for 23 patients (41%) with a median length of stay of 7.5 days (range 2–95 days). Radiation cystitis accounted for a total of 621 inpatient bed days over the 24-month study period. The average running cost of an inpatient hospital bed is €878 (CA$1291) per night.10 This gives a total inpatient care cost of approximately €545,238 (CA$801,908). The cost for a 7.5-day admission was approximately €6585 (CA$9685). See Table 2.
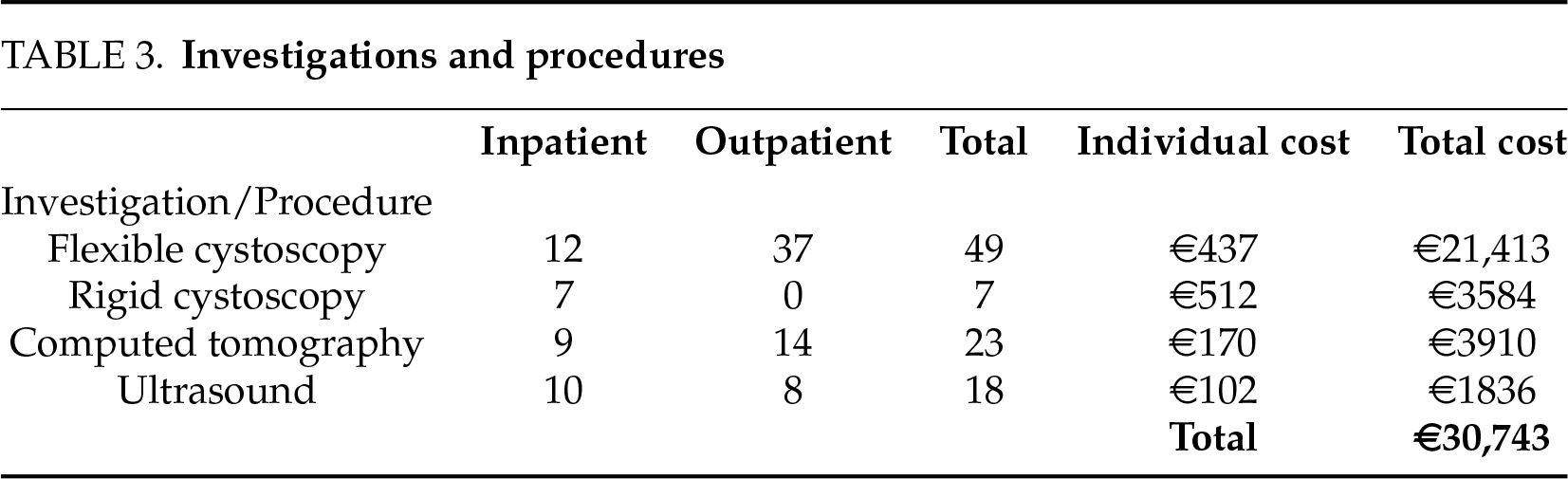
Procedures and investigations
Ninety-eight percent (n = 55) of patients had at least one form of investigation, either as an inpatient or outpatient. Ninety-one percent (n = 51) of patients had at least 1 cystoscopy, either a flexible or rigid cystoscopy. Flexible cystoscopies were performed on 43 patients (77%), with a total of 49 procedures performed. Two patients had 2 flexible cystoscopies and 2 patients had 3 flexible cystoscopies each. Thirty-seven (76%) of these were performed in the outpatient setting and twelve during inpatient admission (24%). The approximate cost for a flexible cystoscopy was €437 (CA$643) at the time of the study9 giving a total estimated cost of €21,413 (CA$31,493) (Table 3). The cost of an individual computed tomography scan is €170 (CA$250), and an ultrasound is €102 (CA$150), according to figures from the hospital finance department (Table 3). Twenty-three computed tomography scans were performed (14 (61%) outpatient, 9 (39%) inpatient) with an approximate total cost of €3910 (CA$5751) (Table 3). Eighteen ultrasound kidneys were performed (8 (44%) outpatient, 10 (56%) inpatient) with an approximate total cost of €1836 (CA$2700) (Table 3). A total of seven patients required a general anesthetic each for rigid cystoscopy and washout during their inpatient stay. The approximate cost of this procedure if performed as a day case is €512 (CA$753),9 costing approximately €3584 (CA$5271) (Table 3).
Radiation cystitis background and demographics
External beam radiotherapy is a commonly utilized treatment modality in pelvic malignancies including cervical, prostate, colorectal, and bladder cancers.2 RC is a well-known and challenging complication of pelvic radiotherapy. Recent innovations in radiotherapy, such as intensity-modulated radiotherapy, have succeeded in dose-minimisation which has helped to reduce the risk of complications to adjacent organs such as the bladder.11 Despite this RC remains a troubling complication for patients. As can be seen from our data, the disease course is chronic in nature and may be characterized by recurrent presentations with haematuria and prolonged hospital admissions. Patients often require multiple investigations and treatment modalities to resolve an acute presentation.
In the setting of some pelvic malignancies, external beam radiotherapy is the preferred treatment for older or co-morbid patients. For example, radiotherapy can be an alternative treatment in patients with muscle-invasive bladder cancer who are unfit for radical surgery or concurrent chemotherapy, and it can also be effective in helping control bleeding.12 The development of RC in this cohort may contribute to prolonged hospital admission and increased recovery time due to frailty and co-morbidities.6 This is supported by our study where the mean age of patients requiring inpatient admission was 76 years (range 62–90). Of the 23 patients requiring inpatient admission, 15 (65%) were 75 years of age or older. The average length of stay for patients aged 75 years or older was 22.9 days vs. 9.8 days for the less than 75-year-old group. Hospital admission can lead to harm for vulnerable older adults; either harm associated with the condition that led to admission, or with iatrogenic factors such as deconditioning, delirium, or nosocomial infection.13 Many patients’ function at the time of discharge is worse than their baseline activities of daily living function. The risk of decline in function increases markedly with age.14
Treatment and associated challenges
As seen in international data, the barriers faced in the treatment of this challenging condition result in prolonged hospital stays. In practice, patients often require multimodal treatment for curative purposes.2,3,7 This carries with it a significant cost to the healthcare system in both bed days and costs of investigations and interventions. Ninety-eight percent of patients in our study had at least one form of investigation, either as an inpatient or outpatient. The median duration of inpatient hospital stay was 7.5 days which costs approximately €6585 (CA$9685).
As with all chronic conditions, recurrent admissions and medical interventions have an economic impact on the patient and healthcare service. Patients present frequently over the course of their disease. Levenback et al. reported a rehospitalization rate of 33% in their cohort of patients with radiation cystitis following pelvic radiotherapy for cervical cancer, and this readmission occurred at a medial time interval of 3.5 months following discharge.4 The average number of admissions per patient in our cohort over these two years was 1.4 admissions. Of the 23 patients requiring inpatient admission, 3 patients had multiple admissions. One 83-year-old patient was admitted 7 times, staying a total of 87 days. Another 82-year-old was admitted twice but stayed a total of 73 days. The last patient aged 72 years was admitted 5 times, staying a total of 18 days.
There is a vast array of treatment options for radiation cystitis quoted in the literature.3,7 Despite this, there is a relative lack of evidence for the efficacy of these given the innate difficulty in carrying out randomized controlled trials to compare them. Current strategies include hydration along with clot evacuation and continuous irrigation, cystoscopic fulguration, intravesical therapies (alum, hyaluronic acid, aminocaproic acid), and hyperbaric oxygen therapy (HBOT), with cystectomy and urinary diversion as a last resort.3,7 Liposomal tacrolimus is a promising new immunosuppressive agent for RC.3
HBOT has been reported as a “game-changer” in the management of radiation cystitis. Some studies reference rates of cure as high as 92%, however, results are highly variable.15 The main benefit is its non-invasive nature; however, it does require repeated sessions (35–50 sessions) of approximately 100 min each. HBOT is not widely available, therefore patients often require accommodation close to the hospital or an inpatient bed for the duration of their treatment. This poses a potentially significant financial burden on the healthcare system.
Economic burden of the disease
Our results detail the financial impact of acute RC presentations and reflect previously published international data. Handmer et al. published a study in 2020 detailing the cost of urologic complications following pelvic radiation therapy.16 Complications following radiotherapy accounted for 3.7% of all urology admissions in 1 year at their center. They reported a combined estimated cost of 1,401,591 Australian dollars (AUD) (CA$1,243,632). However, this is likely a marked underestimation of the total cost. Their study looked at all urologic complications following radiotherapy excluding radiation-related fistulae. Our study looks at RC alone.
Kiechle et al. specifically investigated the economic impact of radiation cystitis in their U.S. institution over four years.17 As was similar in our institution the average patient age was 73.9 years. They estimated the mean cost of an inpatient hospital stay per patient at 11,100 United States dollars (USD) (CA$15,075) when an inpatient cystoscopic procedure was performed. This number increased to USD 16,644 (CA$22,605) when a nephrostomy was inserted for urinary diversion purposes.17
Our research highlighted the significant financial burden posed to our 521-bed tertiary referral center from RC with a total estimated cost of €545,238 (CA$801,908) over these two years for inpatient care alone. This figure likely grossly underestimates the overall costs including outpatient services provided to patients with radiation cystitis-related presentations.
Limitations and strengths of this study
This study is one of few studies to investigate the financial impact of RC on healthcare services. It is the only paper to estimate the cost burden of RC in the Irish Healthcare System. All costs were determined following official quotes from the hospital finance department and using publicly available data from the Healthcare Pricing Office (HPO) to ensure they were as accurate and as up-to-date as possible. Patients with hemorrhagic cystitis are usually initially managed with continuous bladder irrigation and manual washouts. The economic burden of such is difficult to assess and not captured in our data. Our costs are likely an underestimation of the true financial burden as we did not evaluate after-care, and rehabilitation or include costing of some outpatient treatments such as HBOT.
The use of the HIPE coding system facilitated a hospital-wide assessment of this particular condition and its prevalence within our institution. However, there is a risk that due to incorrect coding, some patients may have been missed in our data collection. Finally, this study only captures patients with visible and non-visible haematuria presenting to the hospital for inpatient care or to the outpatient department for investigations; therefore does not reflect the actual burden of radiation cystitis in the community.
Radiotherapy is a widely used treatment modality for pelvic malignancies. It can be utilized as a primary treatment modality or an adjunct to other surgical and medical treatments. Complications from radiotherapy can be costly to the healthcare system. Although complications from radiotherapy are common, it is still a necessary treatment for many patients, and it has been shown to have a positive impact on survival across a wide variety of malignancies. It is our duty as healthcare professionals to recognize complications, manage these complications, and aim to reduce complications through continued research and development. Without further research into the prevention and treatment of this troublesome complication, it will continue to have a significant impact on patients and our healthcare system.
Radiation cystitis accounts for a significant amount of inpatient bed days. A conservative estimate of the overall cost burden exceeds €280,000 (CA$411,810) per year. This is a gross underestimation of the cost burden of radiation cystitis. Improved data collection with accurate coding of conditions and the move towards electronic patient records will help us understand more about complications, the impact on patients, and the economic impact on the healthcare service.
Acknowledgement
I would like to thank the coding and financial departments of University Hospital Galway for providing the data and costings used in this research.
Funding Statement
The authors received no funding for this study.
Author Contributions
The authors confirm contribution to the paper as follows: study conception and design: Brian Gilmartin, Sorcha O’Meara, Michelle Horan, Frank T. D’Arcy and Catherine M. Dowling; data collection: Brian Gilmartin and Sorcha O’Meara; analysis and interpretation of results: Brian Gilmartin and Sorcha O’Meara; draft manuscript preparation: Brian Gilmartin, Sorcha O’Meara, Michelle Horan, Frank T. D’Arcy and Catherine M. Dowling. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials
The data that supports the findings of this study is available from the corresponding author upon reasonable request.
Ethics Approval
Ethical approval was granted by the Clinical Research Ethics Committee of University Hospital Galway (Ref.: C.A. 2864). This retrospective study was exempt from informed consent requirements as all data were anonymized.
Conflicts of Interest
The authors declare no conflicts of interest to report regarding the present study.
References
1. Catalona WJ, Han M. Definitive therapy for localized prostate cancer: an overview. In: Campbell-Walsh urology. Vol. 1. 10th ed. Philadelphia, PA: USA: Elsevier Saunders; 2012. p. 2932–2946. [Google Scholar]
2. Browne C, Davis NF, Mac Craith E et al. A narrative review on the pathophysiology and management for radiation cystitis. Adv Urol 2015;2015(1):346812. [Google Scholar] [PubMed]
3. Li KD, Jones CP, Hakam N et al. Haemorrhagic cystitis: a review of management strategies and emerging treatments. BJU Int 2023;132(6):631–637. [Google Scholar] [PubMed]
4. Levenback C, Eifel PJ, Burke TW, Morris M, Gershenson DM. Hemorrhagic cystitis following radiotherapy for stage Ib cancer of the cervix. Gynecol Oncol 1994;55(2):206–210. [Google Scholar] [PubMed]
5. Denton AS, Clarke NW, Maher EJ. Non-surgical interventions for late radiation cystitis in patients who have received radical radiotherapy to the pelvis. Cochrane Database Syst Rev 2002;2002(3):CD001773. [Google Scholar] [PubMed]
6. Lee V, An Y, Park HS, Yu JB, Kim SP, Jairam V. Emergency department visits for radiation cystitis among patients with a prostate cancer history. BJU Int 2022;130(2):208–216. [Google Scholar] [PubMed]
7. D’Amico MJ, Foss H, Uhr A, Rudnick B, Kloniecke E, Gomella LG. Hemorrhagic cystitis: a review of the literature and treatment options. Can J Urol 2022;29(5):11276–11283. [Google Scholar] [PubMed]
8. Ma JL, Hennessey DB, Newell BP, Bolton DM, Lawrentschuk N. Radiotherapy-related complications presenting to a urology department: a more common problem than previously thought? BJU Int 2018;121(S3):28–32. [Google Scholar] [PubMed]
9. Healthcare Pricing Office, Health Service Executive. DRG Prices for Inpatients and Daycases, ABF 2019 Admitted Patient Price List. Dublin. HSE. Healthcare Pricing Office, HSE. 2019 [Internet]. [cited 2025 Jun 24]. Available from: https://assets.hse.ie/media/documents/2019-admitted-patient-price-list-summary-daycase_plRNppu.pdf. [Google Scholar]
10. Department of Health. Sepsis Management for Adults (including maternityNational Clinical Guideline No. 26, 2021 [Internet]. [cited 2025 Jun 24]. Available from: https://www.lenus.ie/bitstream/handle/10147/630451/Summary%20document.pdf. [Google Scholar]
11. Sveistrup J, af Rosenschold PM, Deasy JO et al. Improvement in toxicity in high risk prostate cancer patients treated with image-guided intensity-modulated radiotherapy compared to 3D conformal radiotherapy without daily image guidance. Radiat Oncol 2014;9(1):44. [Google Scholar] [PubMed]
12. van der Heijden AG, Bruins HM, Carrion A et al. European association of urology guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2025 guidelines. Eur Urol 2025;87(5):582–600. [Google Scholar] [PubMed]
13. Dharmarajan K, Swami S, Gou RY, Jones RN, Inouye SK. Pathway from delirium to death: potential in-hospital mediators of excess mortality. J Am Geriatr Soc 2017;65(5):1026–1033. [Google Scholar] [PubMed]
14. Covinsky KE, Palmer RM, Fortinsky RH et al. Loss of independence in activities of daily living in older adults hospitalized with medical illnesses: increased vulnerability with age. J Am Geriatr Soc 2003;51(4):451–458. [Google Scholar] [PubMed]
15. Pereira D, Ferreira C, Catarino R et al. Hyperbaric oxygen for radiation-induced cystitis: a long-term follow-up. Actas Urol Esp 2020;44(8):561–567. [Google Scholar] [PubMed]
16. Handmer M, Martin J, Tiu A. Costing urologic complications following pelvic radiation therapy. Urology 2020;140:64–69. [Google Scholar] [PubMed]
17. Kiechle JE. Economic burden associated with hospitalization for radiation cystitis: results from a statewide inpatient database. Urol Pract J 2016;3(6):437–442. [Google Scholar]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools