 Open Access
Open Access
HOW I DO IT
Freehand transperineal prostate biopsy under local anesthesia using a novel needle guide system with angle-adjustment feature
1 Department of Urology, Faculty of Medicine, Ankara University, Ankara, 6810, Turkiye
2 Department of Urology, University of Health Sciences, Ankara Dr. Abdurrahman Yurtaslan Training and Research Hospital, Ankara, 6810, Turkiye
* Corresponding Author: Eriz Özden. Email:
(This article belongs to the Special Issue: Advancing Early Detection of Prostate Cancer: Innovations, Challenges, and Future Directions)
Canadian Journal of Urology 2025, 32(5), 477-482. https://doi.org/10.32604/cju.2025.067507
Received 05 May 2025; Accepted 06 August 2025; Issue published 30 October 2025
Abstract
Overview: Freehand transperineal prostate biopsy (TPPB) needle guides are designed to maintain a parallel alignment between the co-axial introducer needle and the ultrasound (US) transducer. However, this parallel alignment necessitates transducer angulations within the patient’s rectum for sampling anterior or posterior regions of the prostate, which introduces several problems both for the patient and the operator. This article introduces a technique using a TPPB needle guide system with a novel angle-adjustment feature, which minimizes intrarectal transducer movements. Objectives: Freehand TPPB typically requires anterior or posterior angulation of the ultrasound (US) transducer, which leads to prostate compression, increased patient discomfort, reduced sonographic image quality, and challenges in MRI-ultrasound fusion biopsy registration. To address these issues, a novel TPPB needle guide system (PERINO-FLEX) featuring a co-axial needle angle adjustment mechanism has been introduced. The system includes a rotating component through which the coaxial needle passes, enabling up to 45 degrees of anterior or posterior angulation within the perineum, without the need to angulate the intrarectal US transducer. In this article, we aim to describe the TPPB technique utilizing this unique angle-adjustment feature and to highlight its advantages.Keywords
Supplementary Material
Supplementary Material FileTransperineal prostate biopsy (TPPB) has gained increasing preference due to its lower risk of infection and antibiotic stewardship, particularly with the adoption of the co-axial biopsy technique. This technique enables comprehensive prostate sampling through a co-axial needle with only two perineal needle entry points and can be performed under local anesthesia.1–4 Freehand TPPB techniques under local anesthesia using a coaxial needle can be classified into two main categories:
1. Needle guide-assisted (freehand) technique: In this approach, the ultrasound (US) transducer is freely manipulated by the operator, and a needle guide is used to direct the biopsy needle.
2. Double freehand technique: Both the US transducer and biopsy needle are independently maneuvered by hand, without the use of a needle guide.4
In the literature, the needle guide-assisted technique is generally referred to as the “freehand” or “single freehand” technique, while the double freehand technique is variably termed “double freehand,” “true freehand,” or “freehand without a needle guide”.5–7 In the double freehand technique, the biopsy needle can be freely oriented by hand, allowing easier access to both anterior and posterior prostate regions without intrarectal transducer tilting. However, aligning the transducer’s imaging plane with the biopsy needle’s axis and continuous visualization of the needle from the perineal skin to the prostate apex is challenging without the aid of a needle guide.2,8 Transperineal needle guides are used to preserve alignment between the needle and the US transducer. These guides maintain the needle aligned in a plane parallel to the transducer, and the biopsy technique is called the freehand TPPB.9 However, this parallel configuration requires the US transducer to be angulated within the rectum to appropriately target the anterior and posterior prostate regions.10 These intrarectal US transducer angulation maneuvers pose several challenges, such as compressing and distorting the prostate, degrading sonographic image quality, hindering MRI-ultrasound fusion for targeted biopsy, and most importantly, increasing patient discomfort.4,5,11,12
To overcome these problems, an innovative TPPB needle guide system (PERINO-FLEX, Geotek, Turkiye) has been recently introduced to the market. This disposable needle guide system incorporates a novel angle-adjustment mechanism that enables anterior and posterior angulations of the co-axial introducer needle without requiring intrarectal tilting of the US transducer. Here, we present the TPPB technique using the angle-adjustable needle guide, highlighting its features and potential advantages of the system.
Ethical approval was obtained from the Ethics Committee of the University of Health Sciences, Ankara Dr. Abdurrahman Yurtaslan Training and Research Hospital, Ankara, Turkiye (Reference number: 2023-12/521). Informed consent was obtained from the patient.
The patient was a 62-year-old male with a total PSA level of 7.2 ng/mL and a prostate volume of 55 mL, as calculated by MRI. His multiparametric prostate MRI was reported as consistent with PI-RADS 2; however, due to a rising PSA level, a decision was made to perform a systematic biopsy by his urologist.
Details of portions of procedure
The classical freehand TPPB procedure using the co-axial technique involves selecting a single puncture site on each side of the perineum, inserting a co-axial introducer needle through the perineum, and subsequently advancing a biopsy needle through the co-axial needle to obtain prostate tissue samples.7 TPPB biopsy with the PERINO-FLEX system follows the same sequence of steps. Unlike conventional needle guides, PERINO-FLEX incorporates a rotating disc-like component with a channel through which the introducer co-axial needle passes (Figure 1). After the co-axial needle is inserted through the channel and the perineum, the rotating disc allows the operator to angle the introducer co-axial needle up to 45 degrees anteriorly or posteriorly within the perineum, without needing to tilt the US transducer inside the rectum (Figure 2A,B). The operator can angulate the intraperineal distal tip of the co-axial or biopsy needles simply by adjusting the proximal end (Figure 2). These angle adjustments enable access to the anterior and posterior regions of the prostate without angulating the US transducer in the rectum (Video 1). During TPPB procedures, tissue samples are obtained from the anterior, mid, and posterior peripheral zones of the prostate.13 One of the main advantages of TPPB over transrectal biopsy is its improved access to the anterior regions of the prostate, which are often undersampled in traditional transrectal approaches, and this makes the anterior angulation maneuver a critical component of freehand TPPB procedures.13,14
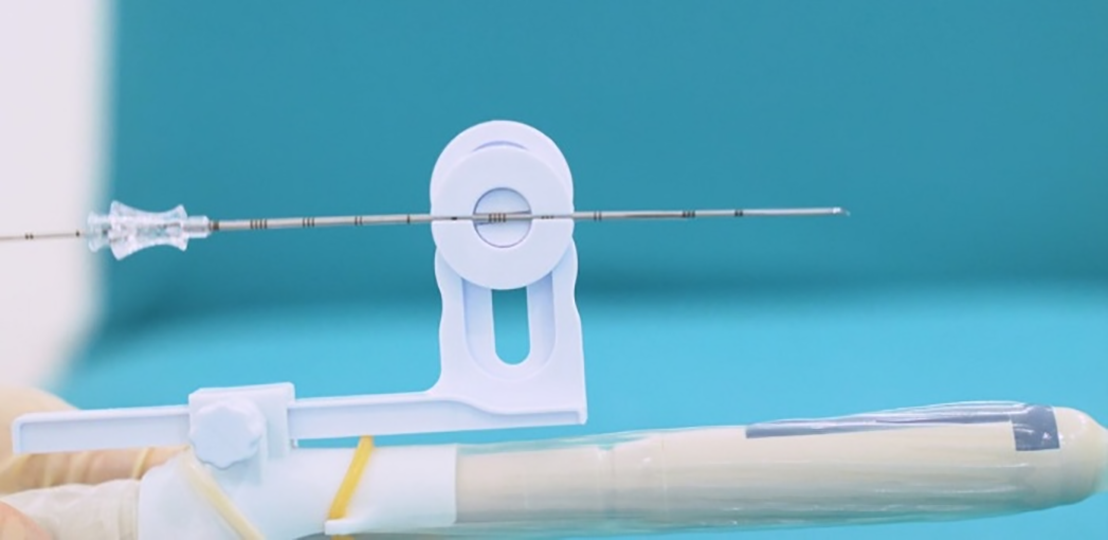
FIGURE 1. Rotating disc with a channel through which the introducer co-axial needle passes
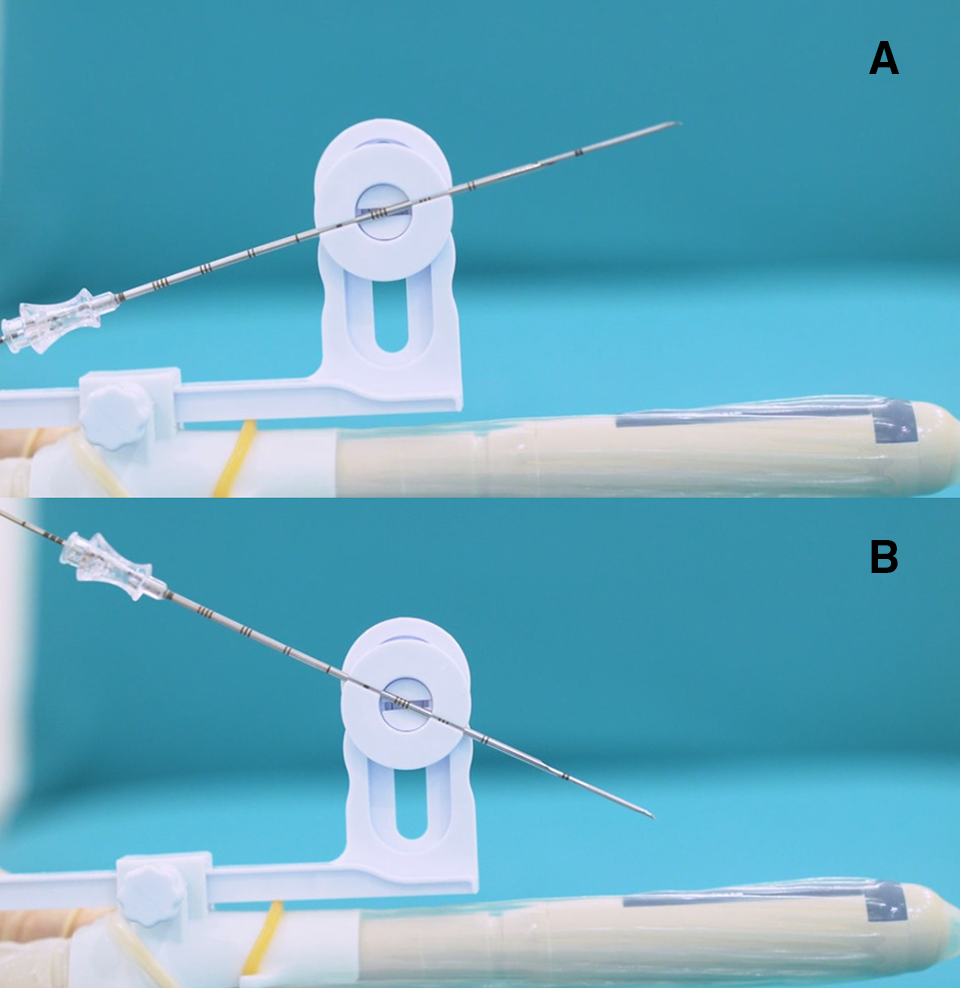
FIGURE 2. Rotating disc. It enables the operator to angulate the co-axial introducer needle up to 45 degrees (A) anteriorly or (B) posteriorly
The biopsy technique progresses through similar stages to TPPB performed using conventional needle guides. Following the application of local anesthesia to the skin, a 15 or 16G co-axial introducer needle is inserted into the perineum through the PERINO-FLEX needle guide at the desired level. As described in previous studies, the tip of the co-axial needle is advanced to approximately 2 cm before the prostatic apex and then halted.2,3,15 The outer end of the co-axial needle, which remains outside the perineum, is directed upward or downward, allowing the inner tip to be oriented toward the desired region of the prostate, without any intrarectal angulation of the US transducer. If necessary, the adjustment screw is used to modify the height of the rotating disc mechanism while the co-axial needle is still inside the perineum (Figure 3A,B). The height-adjustment feature provides a 5 cm range of motion, allowing the operator to move the co-axial needle vertically, facilitated by the relative mobility of the perineal skin and ischiorectal fat. Using these adjustments, systematic peripheral zone biopsies are obtained from the anterior, mid, and posterior regions of the prostate according to the modified Ginsburg protocol.13,15
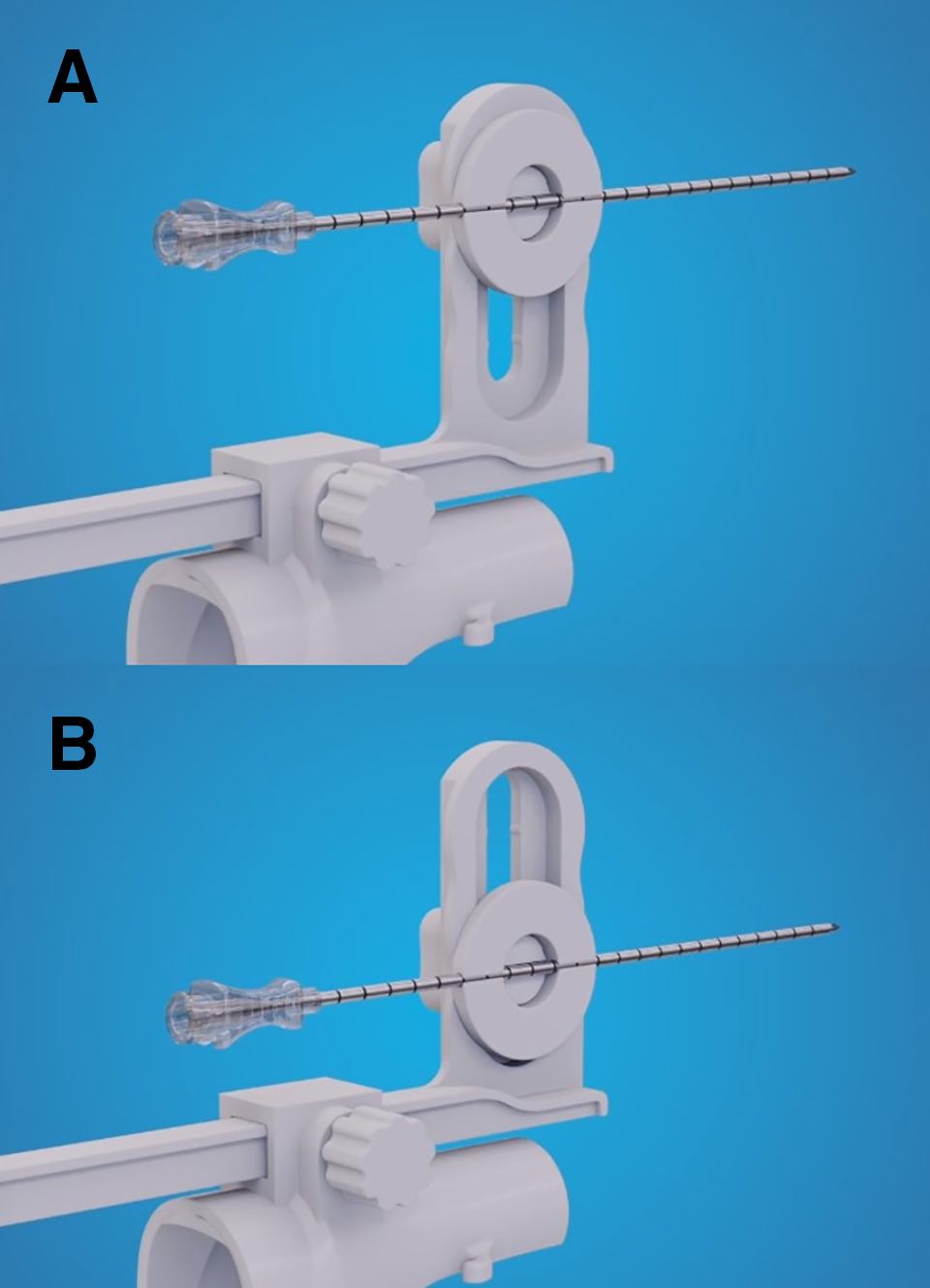
FIGURE 3. Height-adjustment function. It could move the rotating disc-shaped component (A) upward and (B) downward, without adjusting the perineal insertion location of the introducer needle
Management of difficult situations
TPPB can be challenging in cases where the prostate gland is particularly large or when a lesion is located in an extremely anterior position. In such situations, an additional, higher perineal insertion site of the co-axial needle is typically required. However, during biopsy with the PERINO-FLEX system, the operator can adjust the height of the rotating disc-shaped component of the guide upward or downward while the co-axial needle remains inside the perineum. Thus, the height-adjustment feature allows the biopsy needle to reach the extremely anterior regions of large prostates without the need for an additional perineal insertion site (Figure 3A,B). The angle-adjustment feature can also be used to access the anterior regions of the prostate in patients who interference from pubic bone prevents access to the prostate with conventional TPPB needle guides.
The inner tip of the biopsy needle can be directed toward the desired region of the prostate simply by adjusting the proximal end of the needle, allowing precise angulation with only one hand.
As previously mentioned, the clinician may unintentionally distort the prostate while directing the biopsy needle toward the anterior regions, which poses a significant challenge for image registration and biopsy targeting during MRI fusion.11,12 The angle-adjustment feature can simplify registration and image fusion during MRI fusion biopsy by minimizing the need for transducer angulations. The rotation of the disc can be locked using a knob, allowing to preserve a stable needle trajectory for additional samples from the same region. This improved stability also has the potential to enhance the effectiveness of MRI fusion biopsies and MRI-guided focal ablation therapies.
Brief Discussion of the Results
In double freehand TPPB, manual control of the biopsy needle offers the advantage of flexible navigation toward both anterior and posterior prostate zones, eliminating the need to tilt the transrectal US transducer, but despite this flexibility, consistent alignment between the needle trajectory and the ultrasound imaging plane remains technically difficult without a guiding mechanism.2,8 TPPB needle guide systems ensure that the needle remains in a fixed plane relative to the transducer; however, achieving optimal access to anterior and posterior regions with needle guides necessitates tilting the US transducer within the rectum to match the required needle angle.9,10 Such intrarectal adjustments pose some problems. During transducer angulation for anterior prostate sampling, the prostate is inevitably pushed anteriorly and compressed by the transducer.4 This compression can distort the prostate, reduce sonographic image quality, and complicate registration and biopsy targeting during magnetic resonance imaging (MRI) fusion biopsy.11,12 Conversely, when the transducer is angulated posteriorly to obtain posterior prostate samples, the increased distance between the transducer and the prostate surface may degrade sonographic image quality. In patients with large prostates or extremely anterior lesions, the limited anterior mobility of the co-axial needle may necessitate an additional perineal entry site during the biopsy procedure. Most importantly, excessive tilting of the transducer within the rectum or additional perineal entries increase patient discomfort, which cannot be fully alleviated by local anesthesia.4,5 The angle adjustment feature of the PERINO-FLEX needle guide system permits free angulation of the co-axial introducer needle within the perineum, as in the double freehand approach, while preserving alignment with the US transducer, characteristic of the single freehand method. The main distinguishing feature of the PERINO-FLEX system compared to conventional fixed-angle needle guides is its angle-adjustment capability. This novel mechanism enables the operator to direct the biopsy needle toward both anterior and posterior regions of the prostate without requiring intrarectal tilting of the ultrasound transducer. Additional technical advantages include a height-adjustment feature that allows a 5 cm vertical motion range for positioning of the needle entry point into the perineum, independent of fixed, pre-set millimetric intervals. Another distinguishing feature is the ability to lock the rotation of the disc using a knob, which stabilizes the angle of the co-axial needle and allows for repeated biopsies from the same location within the prostate. This angle-stabilization capability is a key advantage of the PERINO-FLEX system over the double-freehand biopsy technique. In the double-freehand approach, the absence of a stabilizing needle guide prevents the operator from consistently targeting the same area of the gland. The double-freehand technique presents another technical challenge: inadvertent retraction of the co-axial needle from the perineum during withdrawal of the biopsy needle through it. The PERINO-FLEX system overcomes this issue with a specially designed channel that prevents unintended forward or backward movement of the co-axial needle, while still permitting controlled adjustments when desired by the operator.
Angle-adjustment feature of this novel needle guide system simplifies the biopsy procedure by eliminating intrarectal transducer angulations and reducing prostate compression, and has the potential to lower perceived patient discomfort and shorten biopsy procedure times. This needle guide incorporating the angle-adjustment feature was first introduced in a recent research article and evaluating the differences between the PERINO-FLEX system and both fixed-angle needle guides and the double-freehand technique in terms of efficiency, cost and technical feasibility remains within the scope of future research.16 The actual impact of the angle-adjustment feature on these outcomes should be validated through future clinical studies.
PERINO-FLEX needle guide system incorporates a novel angle-adjustment mechanism that enables anterior and posterior angulations of the co-axial introducer needle inside the perineum, without requiring intrarectal tilting of the US transducer. As seen in the Video 1, the angulation feature simplifies reaching the desired regions within the prostate gland during local anesthetic freehand TPPB performed with the co-axial technique. Reducing transducer angulations also has the potential to decrease patient discomfort and biopsy procedure times.
Acknowledgement
No acknowledgement to include.
Funding Statement
Not applicable.
Author Contributions
The authors confirm contribution to the paper as follows: Study conception and design: Eriz Özden. Draft manuscript preparation: Eriz Özden, Erdem Öztürk. Literature review: Eriz Özden. Biopsy procedure and video recording: Erdem Öztürk. Critical revision of important scientific content: Eriz Özden, Erdem Öztürk. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval
Ethics committee approval was granted by the Ethics Committee of the University of Health Sciences, Ankara Dr. Abdurrahman Yurtaslan Training and Research Hospital, Ankara, Turkiye (Reference number: 2023-12/521). Informed consent was obtained from the patient.
Conflicts of Interest
The corresponding author (Eriz Özden) is the inventor of the PERINO-FLEX needle guide system and also the co-patent holder of this needle guide. Second author (Erdem Öztürk) declares no conflicts of interest to report regarding the present study.
Supplementary Materials
The supplementary material is available online at https://www.techscience.com/doi/10.32604/cju.2025.067507/s1.
References
1. Grummet J, Gorin MA, Popert R et al. TREXIT 2020: why the time to abandon transrectal prostate biopsy starts now. Prostate Cancer Prostatic Dis 2020;23(1):62–65. doi:10.1038/s41391-020-0204-8. [Google Scholar] [PubMed] [CrossRef]
2. Babaei Jandaghi A, Habibzadeh H, Falahatkar S, Heidarzadeh A, Pourghorban R. Transperineal prostate core needle biopsy: a comparison of coaxial versus noncoaxial method in a randomised trial. Cardiovasc Intervent Radiol 2016;39(12):1736–1742. doi:10.1007/s00270-016-1437-8. [Google Scholar] [PubMed] [CrossRef]
3. Stefanova V, Buckley R, Flax S et al. Transperineal prostate biopsies using local anesthesia: experience with 1,287 patients. prostate cancer detection rate, complications and patient tolerability. J Urol 2019;201(6):1121–1126. doi:10.1097/ju.0000000000000156. [Google Scholar] [PubMed] [CrossRef]
4. Chiu PK, Lo KL, Teoh JY et al. Sectoral cancer detection and tolerability of freehand transperineal prostate biopsy under local anaesthesia. Prostate Cancer Prostatic Dis 2021;24(2):431–438. doi:10.1038/s41391-020-00293-1. [Google Scholar] [PubMed] [CrossRef]
5. Kaneko M, Medina LG, Lenon MSL et al. Transperineal magnetic resonance imaging/transrectal ultrasonography fusion prostate biopsy under local anaesthesia: the ‘double-freehand’ technique. BJU Int 2023;131(6):770–774. doi:10.1111/bju.15985. [Google Scholar] [PubMed] [CrossRef]
6. Ozden E, Ozturk E, Turgut AT. Freehand versus grid-based transperineal prostate biopsy: a comparison of anatomical region yield and complications. Letter. J Urol 2023;210(2):248–249. doi:10.1097/ju.0000000000003546. [Google Scholar] [PubMed] [CrossRef]
7. Chung Y, Hong SK. Shifting to transperineal prostate biopsy: a narrative review. Prostate Int 2024;12(1):10–14. doi:10.1016/j.prnil.2023.11.003. [Google Scholar] [PubMed] [CrossRef]
8. Kanagarajah A, Hogan D, Yao HH, Dundee P, O’Connell HE. A systematic review on the outcomes of local anaesthetic transperineal prostate biopsy. BJU Int 2023;131(4):408–423. doi:10.1111/bju.15906. [Google Scholar] [PubMed] [CrossRef]
9. Recommendations | Transperineal biopsy for diagnosing prostate cancer | Guidance | NICE [Internet]. NICE; 2023. [cited 2025 Jan 10]. Available from: https://www.nice.org.uk/guidance/dg54/chapter/1-Recommendations8. [Google Scholar]
10. Phal PM, Brooks DM, Wolfe R. Sonographically guided biopsy of focal lesions: a comparison of freehand and probe-guided techniques using a phantom. Am J Roentgenol 2005;184(5):1652–1656. doi:10.2214/ajr.184.5.01841652. [Google Scholar] [PubMed] [CrossRef]
11. Fletcher P, De Santis M, Ippoliti S et al. Vector prostate biopsy: a novel magnetic resonance imaging/ultrasound image fusion transperineal biopsy technique using electromagnetic needle tracking under local anaesthesia. Eur Urol 2023;83(5):249–256. doi:10.1016/j.eururo.2023.04.038. [Google Scholar] [PubMed] [CrossRef]
12. Lopez JF, Campbell A, Omer A et al. Local anaesthetic transperineal (LATP) prostate biopsy using a probe-mounted transperineal access system: a multicentre prospective outcome analysis. BJU Int 2021;128(3):311–318. doi:10.1111/bju.15337. [Google Scholar] [PubMed] [CrossRef]
13. Hansen N, Patruno G, Wadhwa K et al. Magnetic resonance and ultrasound image fusion supported transperineal prostate biopsy using the ginsburg protocol: technique, learning points, and biopsy results. Eur Urol 2016;70(2):332–340. doi:10.1016/j.eururo.2016.02.064. [Google Scholar] [PubMed] [CrossRef]
14. Hogenhout R, Remmers S, van Leenders GJLH, Roobol MJ. The transition from transrectal to transperineal prostate biopsy without antibiotic prophylaxis: cancer detection rates and complication rates. Prostate Cancer Prostatic Dis 2023;26(3):581–587. doi:10.1038/s41391-022-00641-3. [Google Scholar] [PubMed] [CrossRef]
15. Zimmerman ME, Meyer AR, Carter HB, Allaf ME, Gorin MA. In-office transperineal prostate biopsy using biplanar ultrasound guidance: a step-by-step guide. Urology 2019;133:247. doi:10.1016/j.urology.2019.07.021. [Google Scholar] [PubMed] [CrossRef]
16. Öztürk E, Özden E, Işikdoğan M et al. The effect of listening to music on pain and anxiety scores during office based transperineal prostate biopsy: a prospective study. Urology 2025;196:254–259. doi:10.1016/j.urology.2024.11.064. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools