 Open Access
Open Access
CASE REPORT
Understanding self-inflicted penile strangulation: a case series analysis of clinical management and psychological considerations
Department of Urology, All India Institute of Medical Sciences, Rishikesh, 249201, India
* Corresponding Author: Vikas Kumar Panwar,. Email:
Canadian Journal of Urology 2025, 32(6), 677-683. https://doi.org/10.32604/cju.2025.063597
Received 18 January 2025; Accepted 13 June 2025; Issue published 30 December 2025
Abstract
Background: Injuries to the penis resulting from self-inflicted strangulation with various objects are uncommon, yet these injuries are more frequently observed in young adults. Medical literature has identified items such as hair, thread, rubber bands, metallic rings, and vacuum erection devices as tools used for this purpose. These constrictive items impede venous return from the penis, potentially leading to severe complications such as ischemia or necrosis. This case series aims to analyse the clinical presentation, management strategies, and psychological dimensions of self-inflicted penile strangulation through a case series. Case Presentation: We conducted a retrospective analysis of three cases of penile strangulation treated at All India Institute of Medical Sciences, Rishikesh between 2022 and 2023. Cases were classified using a modified Bhat et al. grading system. Management techniques, complications, and psychological assessments were documented with a follow-up of 2 years. Individual consent was obtained from the patients for this case series. This article has been prepared according to the PROCESS guidelines. The cases represented a spectrum of clinical severity (Grades I–IV) with diverse constricting devices (metallic ring, plumbing fixtures, hair fibres) and presentation times (6 h to several days). Device-specific removal techniques were employed with successful outcomes. Psychiatric evaluation revealed distinct patterns: sexual experimentation in younger patients (35 and 32 years old) and major depressive disorder with paraphilic tendencies resulting in chronic self-harm (53-year-old), which eventually required partial penectomy. Conclusion: This study underscores the critical need for healthcare providers to recognize and understand the complexities surrounding self-inflicted penile strangulation injuries. By increasing awareness, providers can better address the psychological dimensions and surgical management strategies associated with these cases. Furthermore, involving the family in the patient’s care is essential; counselling and education can play a pivotal role in preventing future recurrences of major depressive disorder.Keywords
Supplementary Material
Supplementary Material FileSelf-inflicted injuries to the penis resulting from strangulation are rare, with only about 60 cases reported to date, primarily documented as case reports.1,2 The presentation of these injuries can be challenging for emergency physicians and necessitates urgent multidisciplinary management involving both urologists and psychiatrists. These occurrences are commonly observed among middle-aged and elderly men.3–5 Various foreign body objects, including hair, thread, rubber bands, and metallic rings, have been reported in the literature for penile strangulation.1,6–8 The motivations behind such self-inflicted injuries can vary significantly, ranging from sexual experimentation to psychiatric conditions.2,9 Herein, we present three distinct case presentations along with their successful management strategies.
Penile strangulation injuries require a prompt, adequate, and multidisciplinary approach. Improper management of penile strangulation can lead to severe complications, including erectile dysfunction, loss of penile skin, penile necrosis, and penile amputation.3 Therefore, healthcare providers must understand the various safe and effective techniques for managing such cases promptly. This case series was conducted to analyze and document instances of self-inflicted penile strangulation, focusing on the motivations, management strategies, and complications.
The study design involved a retrospective review of three cases presented at our institution over a period of 2 years (January 2022 to December 2023) and strictly followed the CARE Case Report Guidelines (see Supplementary Material for the CARE checklist). The study also adhered to the Declaration of Helsinki guidelines. Institutional ethical clearance was obtained for the study from the All India Institute of Medical Sciences Institutional Ethics Committee (IEC) with IEC letter no. AIIMS/IEC/25/25. Informed consent was secured from all patients for the use of their anonymized data in this publication.
Data collection involved a thorough review of patient medical records, including clinical history, physical examination findings, imaging studies, and treatment outcomes. Each case was analysed to identify the type of object used for strangulation, the duration of the injury, the management approach, and any complications encountered.
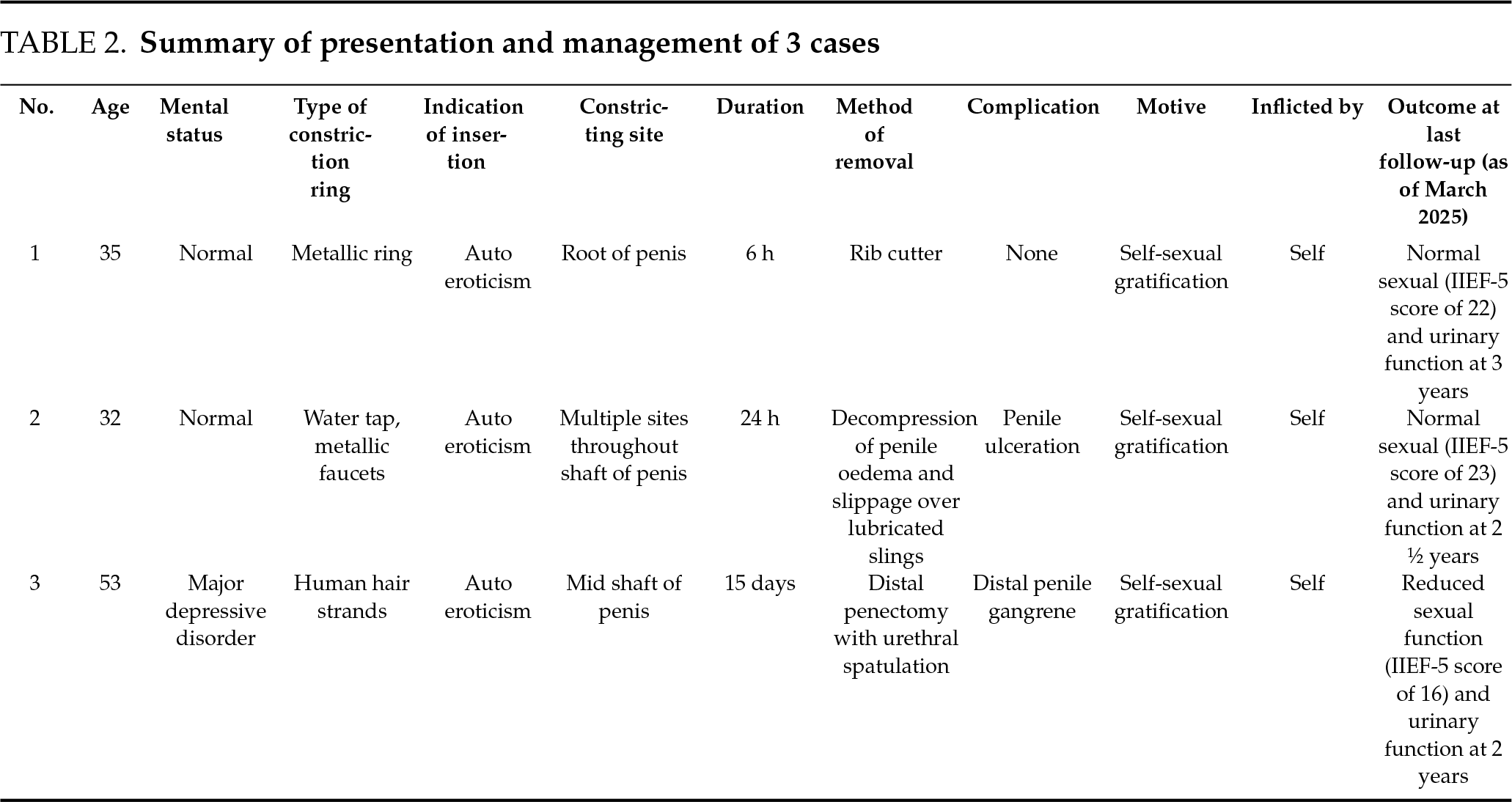
The classification system described by Bhat et al.10 proposes a comprehensive grading system (Table 1) that helps in standardizing the assessment and management, which was used in this study.
The follow-up criteria encompassed a comprehensive evaluation of sexual function utilizing the International Index of Erectile Function (IIEF-5) scoring system, erectile hardness score (EHS), alongside assessments of urinary function through uroflowmetry. Additionally, the prevention of recurrences was a key focus. Follow-up data were systematically collected over six months, with assessments conducted at four-week intervals to evaluate long-term outcomes. Mini-mental state examination (MMSE) was used for cognitive assessment, but no structured psychiatric assessment tool was used, which is a limitation in our study. Furthermore, individualised psychological evaluation and counselling were provided to support the overall well-being of the participants. All data were anonymized to ensure patient confidentiality.
Patient: A 35-year-old male arrived at the emergency department with intense pain and swelling of the penis. He disclosed that he had worn a metallic ring on his penis to enhance sexual activity.
History: The ring had been tightly applied around the base of his erect penis approximately six hours prior. Soon after, he experienced escalating pain and rapid swelling.
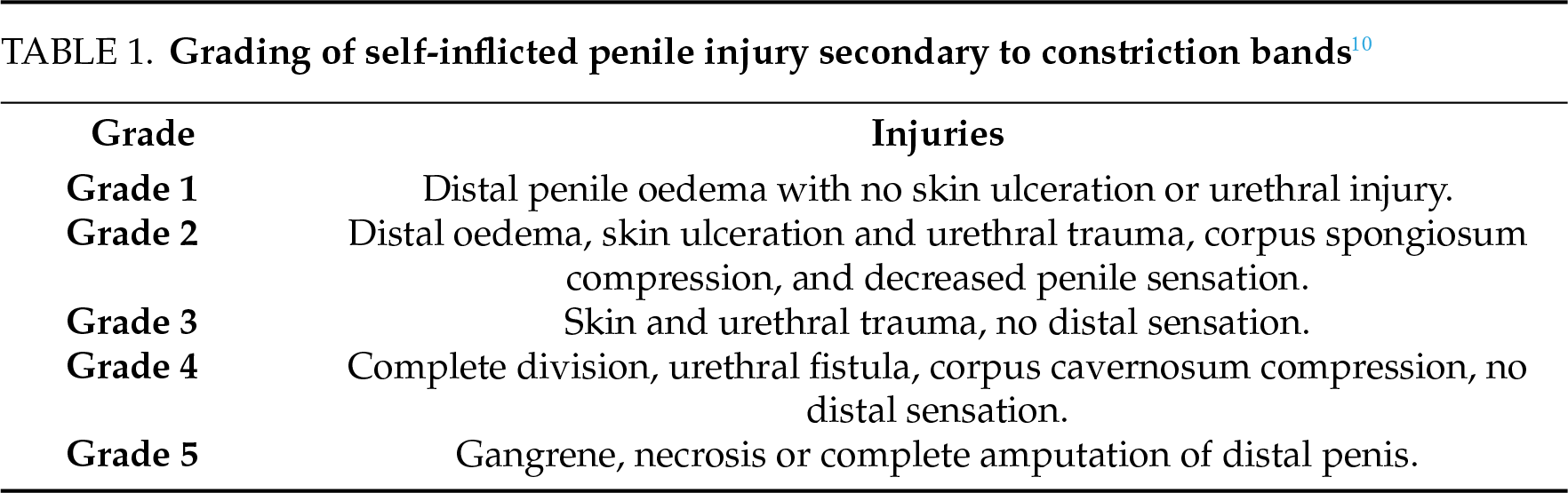
Clinical Findings: Examination revealed considerable swelling and constriction at the level of the ring. The patient exhibited significant distress due to pain (Figure 1).
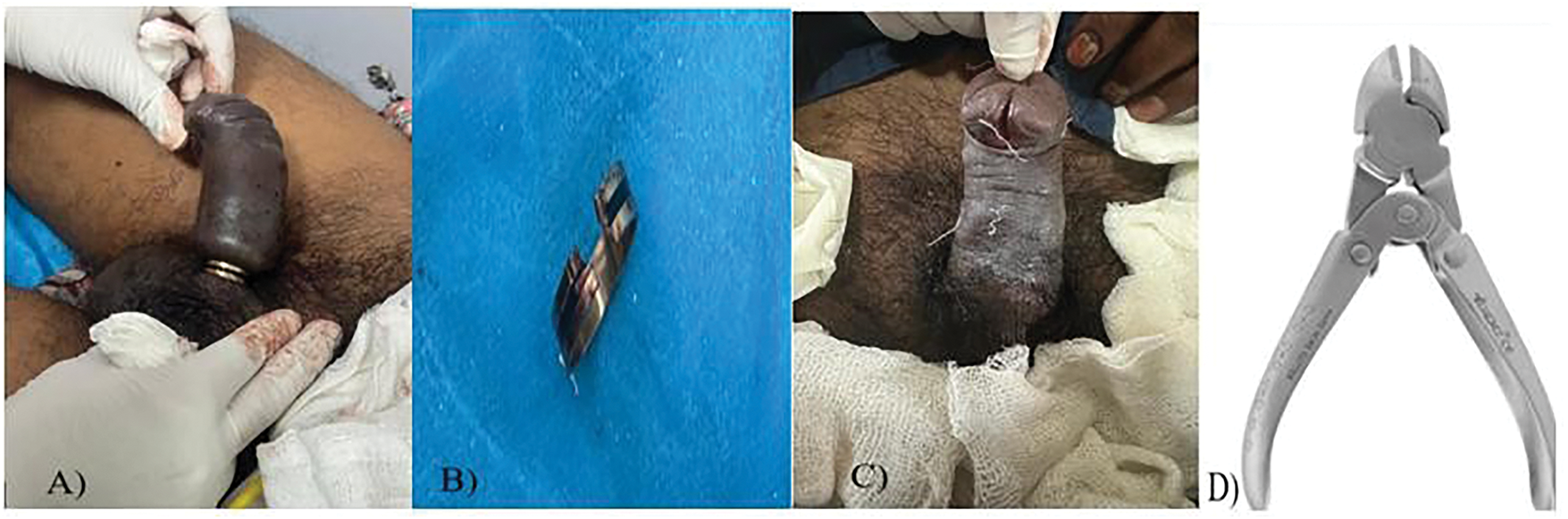
FIGURE 1. Clinical presentation of penile strangulation. (A) Severe penile edema due to constriction. (B) Removed metallic ring. (C) Post-procedure penile appearance. (D) Metallic rib cutter used for removal
Management: Immediate measures were taken to relieve the strangulation. The ring was removed using a metallic rib cutter after placing several slings between the ring and the penile surface for extraction. A 16 Fr urinary catheter was inserted during the procedure, and the patient was discharged with the catheter to be removed five days later. The MMSE indicated normal cognitive function. The patient received counseling on preventing such incidents.
Follow-up: The patient returned for follow-up after catheter removal on day five and reported normal urination without complaints. At six weeks post-treatment, he reported a normal erectile hardness score (EHS).
Patient: A 32-year-old male presented with complaints of gradually worsening pain and swelling of the penis over the past 24 h.
History: He had worn multiple metallic rings from a tap faucet on his penis for sexual enhancement and left it on for 24 h. He delayed seeking medical attention despite increasing discomfort and swelling due to embarrassment.
Clinical Findings: Examination showed significant edema and discoloration distal to the ring, indicating compromised circulation (Figure 2).
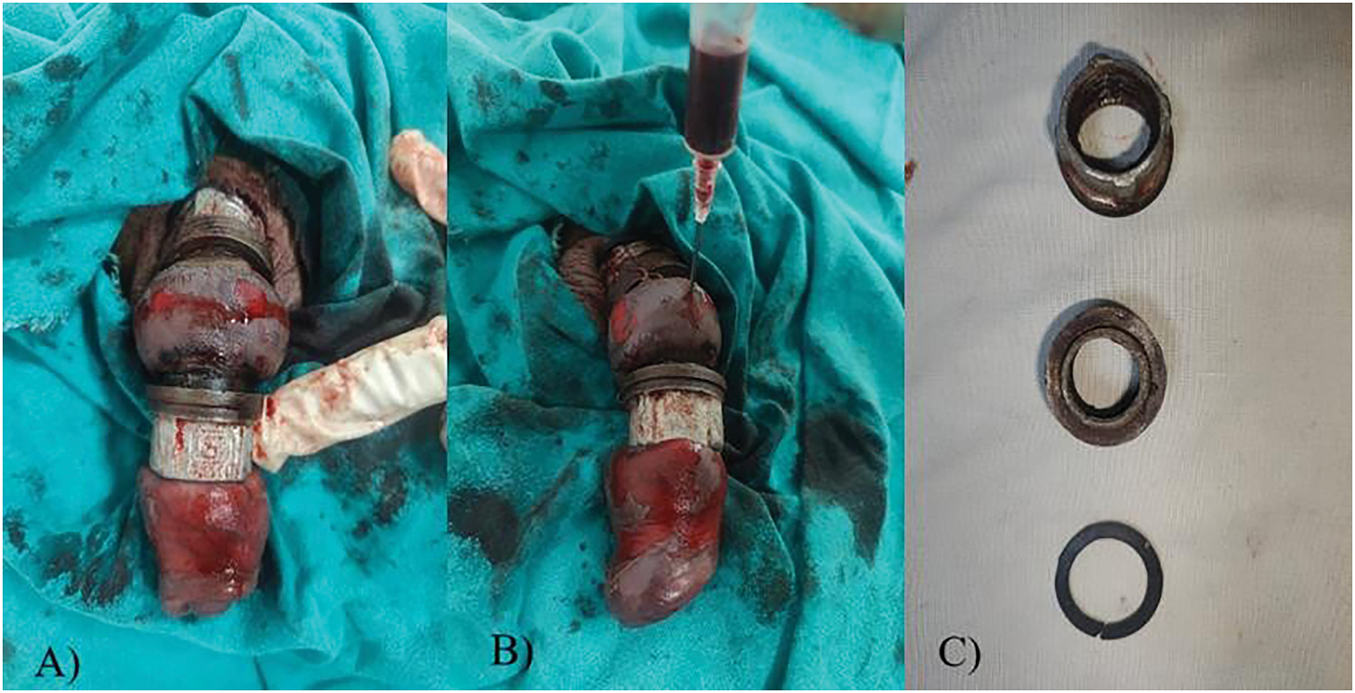
FIGURE 2. Clinical presentation of penile strangulation. (A) Multiple tap faucets are causing penile strangulation. (B) Decompression of penis. (C) Metallic faucets that were removed
Management: Urgent removal of the ring was performed under anesthesia. Urgent decompression of penile strangulation was done with active aspiration and reduction of edema followed by placement of multiple slings between the penis surface and the rings, which were then slipped off slowly with lubrication over the slings. A 16 Fr urinary catheter was inserted with drainage of clear urine. The MMSE showed normal cognitive status. The patient was counseled regarding the prevention of such acts.
Follow-up: The patient was discharged subsequently on a catheter and reviewed after 5 days. Penile skin showed a reduction in edema, a catheter was removed, and the patient voided well. At 6 weeks patient was reviewed again, and he reported no urinary complaints, and EHS was within normal limits.
Patient: A 53-year-old male with major depressive disorder presented with chronic penile pain and an inability to urinate.
History: The patient had tied multiple strands of human hair at the base of his glans penis for 15 days. The patient had used hair strands for auto-eroticism and developed pain and swelling; however, did not seek medical care due to embarrassment.
Clinical Findings: Examination revealed chronic skin changes, tissue fibrosis, and necrosis distal to the ligation site. The patient had developed a urethral fistula proximal to the site of ligation, resulting in urine leakage from an abnormal opening (Figure 3).

FIGURE 3. Hair fibers used for occlusion in the mid-penile shaft region
Management: Surgical intervention was necessary due to the chronic nature of the injury. The patient underwent partial penectomy with dorsal spatulation of the urethra. The distal-most gangrenous segment of the penis was removed and 16 Fr urinary catheter was placed. The patient was diagnosed with major depressive disorder, prompting a psychiatry consultation. Following this assessment, the patient was reinitiated on his medical therapy to address the condition effectively. Additionally, the patient’s family members were counseled and educated to help prevent future recurrences.
Follow-up: The patient was successfully discharged on post-op day 7 with a healthy residual penile stump with a catheter in situ. The patient was reviewed subsequently and the voiding trial was given 2 weeks post-operatively and the patient voided well from the new urethral meatus.
These cases underscore the significance of prompt diagnosis and a holistic management approach, which includes addressing any underlying psychiatric conditions and recognizing the role of family support in mental health management to prevent the recurrence of such types of injuries.
Injuries from penile strangulation, while rare, pose considerable challenges in diagnosis and treatment. The exact incidence of penile strangulation injuries is unknown, and the first case of penile strangulation was reported by Gauthier in 1755.11 Katz et al. reported in their case report that early intervention is crucial for preventing long-term complications.1 The variety of objects used for strangulation necessitates different approaches to management, as highlighted by Noh et al.12 in their modified string method for the removal of constrictive devices. Similarly, we employed different techniques for each case depending on the type and nature of the constricting object.
Literature suggests these cases are often underreported due to the sensitive nature of the incidents and the embarrassment patients may feel.4 The motivations for self-inflicted strangulation can vary widely, with some instances linked to sexual experimentation and others to attempts at managing urinary symptoms, particularly across different cultural backgrounds.2,12–14 In some cultural settings, the use of penile constriction devices may be linked to sexual myths or beliefs regarding the enhancement of erectile function.4 In Taiwan, for example, a practice of Chinese kung fu called Nine-Nine Chi-Gung uses this method to improve sexual function.14
The grading system proposed by Bhat et al.10 has proven invaluable in standardizing the assessment and management of these injuries, allowing for more systematic approaches to treatment (Table 1). Their classification helps in determining the urgency of intervention and the most appropriate treatment modality. The same classification system was used in our study.
Emergency physicians and urologists should be aware of the various techniques for removing constricting objects. Katz et al. advocated a non-invasive “pseudo-pulley” method for the removal of a constricting metallic ring.1 A similar method was used for the removal of the ring in our case 2 (delayed presentation) with the help of multiple slings.
Campbell et al. did a literature review of 56 cases and recommended follow-up after extrication to include sexual function evaluation, AUA symptom score, uroflowmetry, Post Void Residual studies, and cystoscopy if required.13 All the parameters were followed up in our study accordingly, and the results are shown in Table 2.
Psychiatric evaluation should be a routine part of the assessment, particularly for chronic cases or those with underlying mental health conditions.15 Patients should be counseled regarding the risk of using penile constriction devices in the future. If, however, patients are still willing for the same, the use of such devices should be restricted to safer constricting devices and not extend beyond 30 min in order to prevent complications. Other alternative safer methods for sexual satisfaction and erectile function enhancement must be taught and counseled to the patient, along with their partner.2
This study is limited by a small sample size and its retrospective nature, which may restrict the generalizability of the findings. Furthermore, the lack of long-term follow-up data limits our understanding of the psychological and functional outcomes for these patients. Notably, there is a lack of long-term sexual function outcomes, and no standardized psychiatric screening tool was utilized, which could affect the reliability of the results. Additionally, underreporting bias may occur due to the sensitive nature of the condition. Future research should focus on larger, multi-centre prospective cohort studies that incorporate standardized psychological screening to better understand the epidemiology and management of penile strangulation injuries. Investigating the role of psychological interventions in preventing recurrence and improving patient outcomes is also warranted.
This study underscores the critical need for healthcare providers to recognize and understand the complexities surrounding self-inflicted penile strangulation injuries. The cases of penile strangulation detailed in this report illustrate the complexity and potential severity of these injuries. Timely diagnosis and appropriate management are crucial for patient recovery.12 By increasing awareness, providers can better address the psychological dimensions and management strategies associated with these cases. Furthermore, involving the family in the patient’s care is essential; counseling and education can play a pivotal role in preventing future recurrences of self-harm. Limited by 3 cases, however, healthcare providers should be trained in non-invasive and surgical methods of penile ring removal, while also considering psychiatric evaluation as part of post-treatment care.
Acknowledgement
Not applicable.
Funding Statement
There was no funding supplied.
Author Contributions
Siddharta Saxena: Manuscript author, data collection, submission of manuscript and revisions; Vikas Kumar Panwar: Conceptualization, data curation, investigation, methodology, project administration, visualization; Ankur Mittal: Conceptualization, data curation, investigation, methodology, project administration, visualization; Mohammed Taher Mujahid: Data collection, manuscript review, tables/figures preparation and data analysis; Mehul Agarwal: Data collection and analysis; Nalin Kumar Srivastava: Data collection and analysis. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials
The data that support the findings of this case report are available from the corresponding author, Vikas Kumar Panwar, upon reasonable request.
Ethics Approval
The study adhered to the Declaration of Helsinki guidelines. Institutional ethical clearance was taken for the study from the All India Institute of Medical Sciences Institutional Ethics Committee with IEC letter no. AIIMS/IEC/25/25.
Informed Consent
Informed consent was taken from individual patients for the collection of data and the sharing of information.
Conflicts of Interest
The authors declare that this work is original and all sources are acknowledged. The authors declare no conflicts of interest to report regarding the present study. The content of this manuscript has not been published or submitted for publication elsewhere.
Supplementary Materials
The supplementary material is available online at https://www.techscience.com/doi/10.32604/cju.2025.063597/s1.
References
1. Katz DJ, Chin W, Appu S et al. Novel extraction technique to remove a penile constriction device. J Sex Med 2012;9(3):937–940. doi:10.1111/j.1743-6109.2011.02598.x. [Google Scholar] [PubMed] [CrossRef]
2. Silberstein J, Grabowski J, Lakin C, Goldstein I. Penile constriction devices: case report, review of the literature, and recommendations for extrication. J Sex Med 2008;5(7):1747–1757. doi:10.1111/j.1743-6109.2008.00848.x. [Google Scholar] [PubMed] [CrossRef]
3. Ivanovski O, Stankov O, Kuzmanoski M et al. Penile strangulation: two case reports and review of the literature. J Sex Med 2007;4(6):1775–1780. doi:10.1111/j.1743-6109.2007.00601.x. [Google Scholar] [PubMed] [CrossRef]
4. Perabo FG, Steiner G, Albers P, Müller SC. Treatment of penile strangulation caused by constricting devices. Urology 2002;59(1):137. doi:10.1016/s0090-4295(01)01485-6. [Google Scholar] [PubMed] [CrossRef]
5. Patel S, Gupta N, Sharma R et al. Penile strangulation: analysis of postextrication follow-up, management, and outcomes. Am J Mens Health 2023;17(1):15579883231223366. doi:10.1177/15579883231223366. [Google Scholar] [PubMed] [CrossRef]
6. Wang Y, Wang J, Zhang R et al. Vacuum constriction devices for erectile dysfunction: a systematic review and network meta-analysis. Front Endocrinol 2021;12:7844489. doi:10.1038/s41443-025-01102-w. [Google Scholar] [PubMed] [CrossRef]
7. Yildiz S, Gokce MI, Ozdemir E, Gokce A. From entrapment to recovery: resolution of penile strangulation from a double-wall metal ring—A case report and review. J Urol Surg 2025;12(1):1–4. doi:10.4274/jus.galenos.2025.2025-1-12. [Google Scholar] [CrossRef]
8. Jain S, Sood SS, Goel S, Goel SK. Penile strangulation: a case report and review of the literature. Arab J Urol 2020;18(3):224–228. doi:10.1080/2090598X.2020.1796002. [Google Scholar] [CrossRef]
9. Smith J, Brown K, Lee T et al. Penile constriction devices: a randomized survey study to compare preferences between two medical-grade devices. 2023. doi:10.1093/jsxmed/qdae151. [Google Scholar] [CrossRef]
10. Bhat AL, Kumar A, Mathur SC, Gangwal KC. Penile strangulation. Br J Urol 1991;68(6):618–621. [Google Scholar] [PubMed]
11. Gauthier M. Observation of a strangulation of the testicles and the penis, caused by the passage of a lighter. J Med Chir Pharmacol 1755;3(358):1755. doi:10.1016/j.eucr.2023.102382. [Google Scholar] [CrossRef]
12. Noh J, Kang TW, Heo T, Kwon DD, Park K, Ryu SB. Penile strangulation treated with the modified string method. Urology 2004;64(3):591. doi:10.1016/j.urology.2004.04.058. [Google Scholar] [PubMed] [CrossRef]
13. Campbell KJ, Kwenda EP, Bozorgmehri S, Terry RS, Yeung LL. Penile strangulation: analysis of postextrication follow-up, sequelae, and a review of literature. Am J Mens Health 2024;18(1):15579883231223366. doi:10.1177/155798832312233. [Google Scholar] [CrossRef]
14. Chang SJ, Chiang IN, Hsieh JT, Liu SP. Extrication of penile constriction device with corpora aspiration. J Sex Med 2009;6(3):890–891. doi:10.1111/j.1743-6109.2008.01137_1.x. [Google Scholar] [PubMed] [CrossRef]
15. Mani UA, Tripathi P, Sarangan V et al. Penile strangulation. Natl J Emerg Med 2023;1(3):67–70. [Google Scholar]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools