 Open Access
Open Access
CASE REPORT
Pulmonary Hypertension Crisis in Patient with Tetralogy of Fallot and Mixed Total Anomalous Pulmonary Vein Connection after the Primary Correction: A Rare Case Report
1 Department of Anesthesia and Intensive Therapy, National Cardiovascular Center Harapan Kita, Jakarta, Indonesia
2 Doctoral Program, Faculty of Medicine and Public Health, University of Gadjah Mada, Yogyakarta, Indonesia
3 Department of Anesthesia and Intensive Therapy, Universitas Gadjah Mada/Dr. Sardjito Hospital, Yogyakarta, Indonesia
4 Department of Cardiology and Vascular Medicine, Universitas Gadjah Mada/Dr. Sardjito Hospital, Yogyakarta, Indonesia
* Corresponding Author: Lucia Kris Dinarti. Email:
Congenital Heart Disease 2023, 18(6), 671-678. https://doi.org/10.32604/chd.2023.044746
Received 07 August 2023; Accepted 16 October 2023; Issue published 19 January 2024
Abstract
Tetralogy of Fallot (TOF) with total anomalous pulmonary vein connections (TAPVC) is a rare type of complex congenital heart disease among all TOF cases. Co-presentation of major aortopulmonary collateral arteries (MAPCAs) compensates for the lack of central pulmonary blood flow and decreases the severity of right-to-left shunting in TOF. We present a case of a 2-year-old child with complex diagnoses of TOF, TAPVC, a large secundum atrial septal defect (ASD), and intraoperatively identified MAPCAs. She underwent surgery to repair the TAPVC, valve-sparing reconstruction of the right ventricular outflow tract, interventricular defect closure, and the creation of patent foramen ovale (PFO). After the operation, hemodynamic instability happened along with sudden blood pressure drop, desaturation, and increased central venous pressure, which subsided after administering inhalational nitric oxide (NO). A postoperative pulmonary hypertension crisis was suggested when the patient experienced recurrent symptoms after the termination of NO. Echocardiographic findings of a D-shaped left ventricle (LV), right-to-left PFO shunt and high tricuspid valve gradient firmly established the diagnosis. It was subsequently managed with continuous NO inhalation and sildenafil, which rendered a satisfactory outcome. Repaired TOF and TAPVC could be at particular risk of developing pulmonary hypertension crisis, especially in the presence of MAPCAs due to possible remodeling of the pulmonary vasculature. Furthermore, a relatively non-compliant LV function and small left atrial size may exacerbate the risk of developing postcapillary pulmonary hypertension after TAPVC repair. A successful postoperative outcome calls for a meticulous preoperative analysis of the anatomical lesions, as well as careful monitoring.Keywords
Tetralogy of Fallot (TOF) along with total anomalous pulmonary vein connections (TAPVC) is a rare form of congenital heart disease with an incidence of 0.25%–0.35% among all TOF cases [1]. Symptoms of TOF are associated with diminished pulmonary blood flow and low arterial oxygen saturation. In TAPVC, blood from pulmonary veins flows abnormally into the right atrium (RA) via its tributaries. Typically, an atrial septal defect (ASD) exists, allowing blood to pass from the RA to the left atrium (LA) [2]. However, the emergence of major aortopulmonary collateral arteries (MAPCAs) in TOF and TAPVC allows deoxygenated blood to flow through the lungs, compensating for the lack of central pulmonary blood flow and possibly decreasing the severity of right-to-left shunting. In this article, we present a case of a pediatric patient who was diagnosed with a combination of TOF and TAPVC, as well as intraoperatively identified MAPCAs. However, this patient then suffered from a postoperative pulmonary hypertension crisis during intensive care monitoring. Hence, this report aims to describe the rationale behind the development of postoperative pulmonary hypertension, as well as the anesthetic management that contributed to the successful outcome in this patient. We wrote this article in accordance with the CARE case report standards and checklist [3].
A 2-year-old girl who weighed 10 kg presented with symptoms of dyspnea and cyanosis, which were exacerbated by physical activity. The symptoms were alleviated when the patient was performing a squatting position. During physical examination, blood pressure (BP) was 92/66 mmHg, heart rate (HR) 100 bpm, and room air oxygen saturation (SaO2) varied between 62%–69%. Chest radiograph showed cardiomegaly with cardiothoracic ratio of 55%, flat heart waist with downward apex, and oligemic vasculature appearance (Fig. 1).
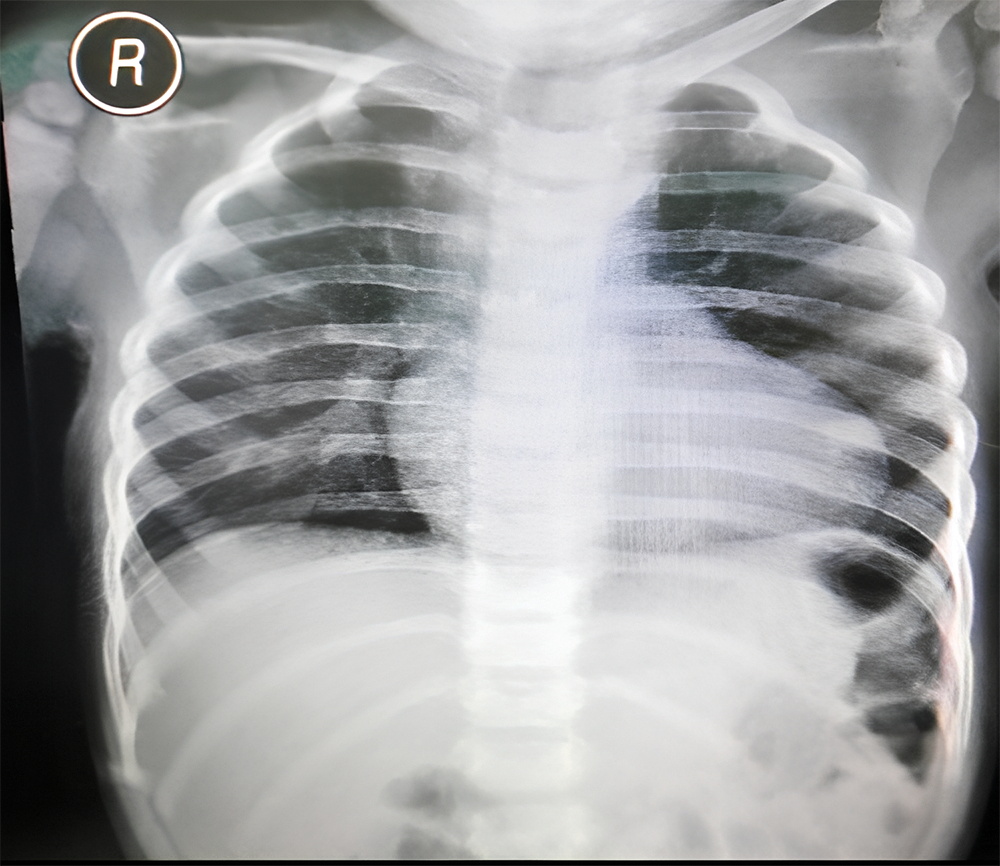
Figure 1: Preoperative chest radiograph revealing cardiomegaly with cardiothoracic ratio 55%, normal aortic segment, flat heart waist, downward apex, and oligemic vasculature appearance
Her clinical characteristics, chest radiograph, and bedside transthoracic echocardiography (Figs. 2A–2C) supported the diagnosis of tetralogy of Fallot (TOF). Additional lesions were also identified, consisting of mixed-type TAPVC with the end of the pulmonary veins connected to the superior vena cava (SVC) and right atrial junction, and a large secundum atrial septal defect (ASD) (Figs. 3A and 3B). The preoperative pressure gradient across the right ventricular outflow tract (RVOT) was 58 mmHg. LA chamber was 17 mm in diameter (z-score < −3 for BSA 0.489 m2), and LV chamber during diastole was 21 mm (z-score < −3 for BSA 0.489 m2) [4]. Additionally, a multi-slice CT scan confirmed the diagnosis of TOF with mixed TAPVC (Fig. 4). The McGoon ratio of this patient was 1.802, which was deemed acceptable for TOF repair. No diagnostic challenges were identified. The patient was then scheduled for total corrective repair for the TAPVC, right ventricular outflow tract and chamber defects reconstruction in TOF, and creation of patent foramen ovale.
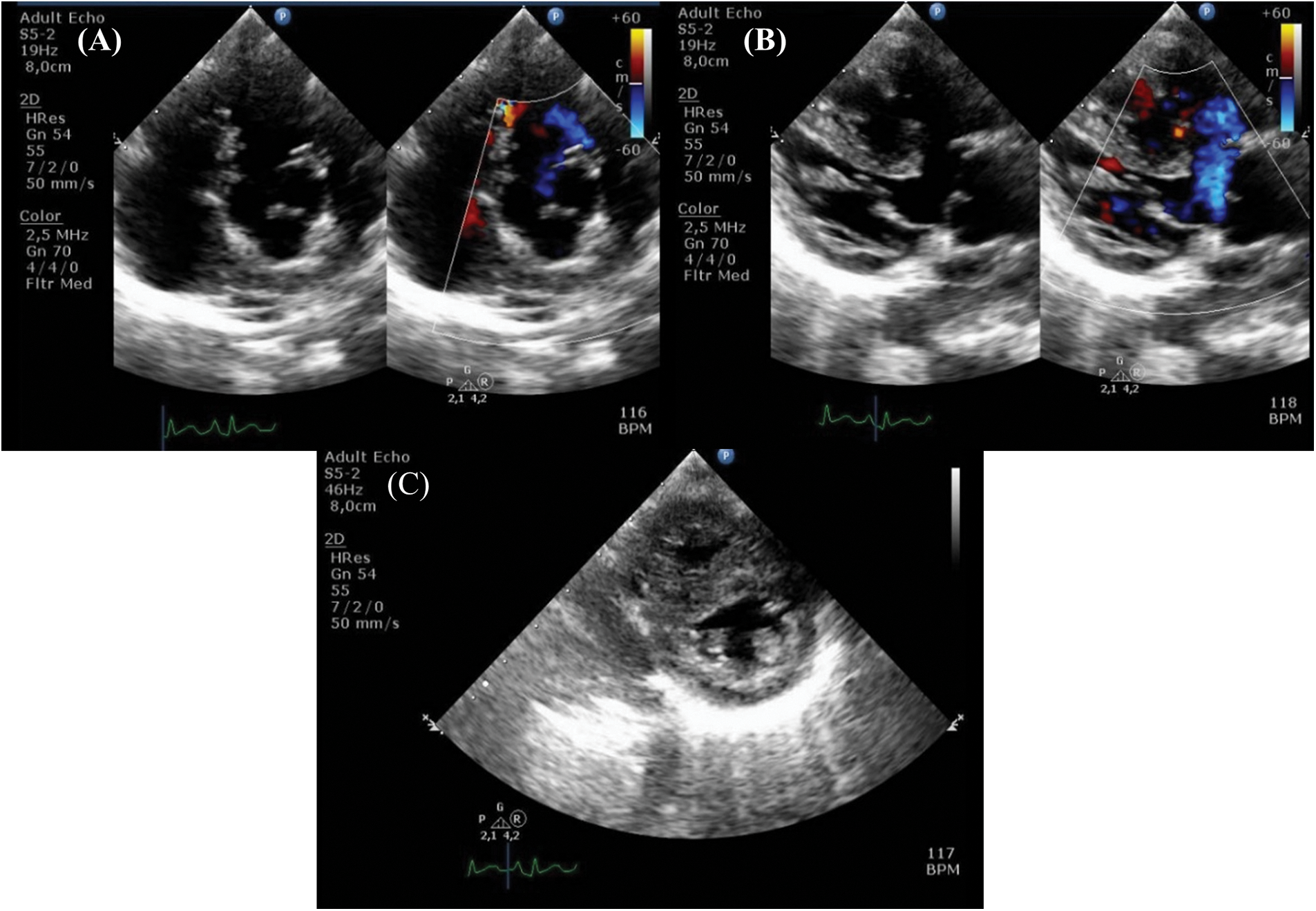
Figure 2: Preoperative echocardiography shows characteristics of tetralogy of Fallot (A) pulmonary stenosis, (B) overriding of the aorta, and (C) right ventricular hypertrophy
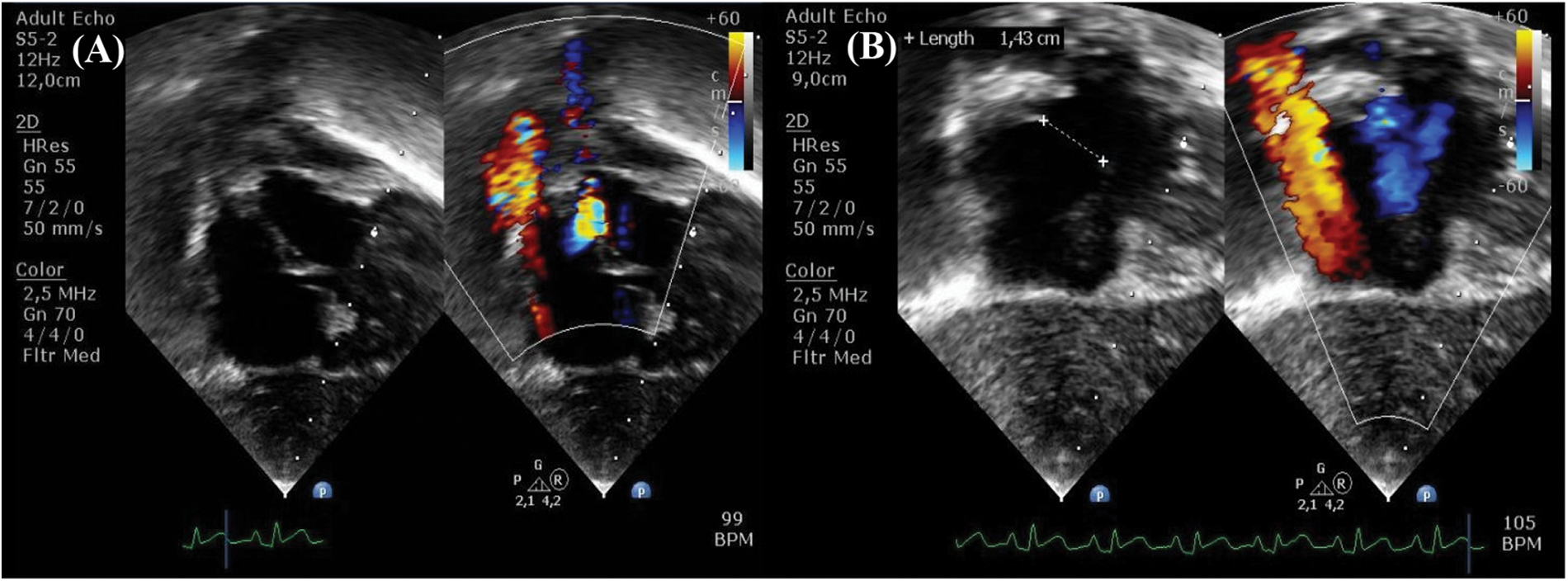
Figure 3: Preoperative echocardiography demonstrates (A) total anomalous pulmonary valve connection with (B) atrial septal defect

Figure 4: Preoperative MSCT shows supra cardiac connection where the two pulmonary veins from each lung converge to common pulmonary vein before joining the superior vena cava (arrow)
In the operating room, the patient was sedatively induced with 1 mg of midazolam, 30 μg of fentanyl, and 2 mg of vecuronium. An arterial line was inserted into the left radial artery, followed by a central venous catheter (CVC) insertion in the right internal jugular vein. A mixture of 50% oxygen and sevoflurane 1 vol% on air, as well as increasing doses of induction agents, were used to maintain a balanced anesthesia. Tidal volume and respiratory rate were also adjusted to maintain stable expired carbon dioxide concentration. During cross-clamping of the aorta, blood was found flowing into the heart chamber, which indicated the presence of major aortopulmonary collateral arteries (MAPCAs). The valve-sparing technique was used by the surgeon, in addition to surgical repair of the anomalous pulmonary veins and the atrial septal defect. The procedures were performed within 142 min. After rewarming, the patient was successfully removed from cardiopulmonary bypass machine (duration: 191 min), and was electively supported with adrenaline 0.1 mcg/kg/min and milrinone 0.375 mcg/kg/min. The vital signs were BP 95/64 mmHg, HR 100 bpm, central venous pressure (CVP) 5 mmHg, and SaO2 100%.
In the postoperative period, the patient was admitted to the intensive care unit (ICU) with stable hemodynamics and blood gas analysis. Twelve hours after admission, blood pressure (BP) dropped to 50/30 mmHg, and CVP increased to 18 mmHg. Simultaneously, arterial blood gas analysis showed mixed acidosis with pCO2 76 mmHg, pO2 57 mmHg and SaO2 85.6%.
Nitric oxide (NO), as a specific pulmonary artery vasodilator, was immediately given for the patient as the symptoms were suggestive of a pulmonary hypertension crisis. 20 ppm of NO was administered along with a bolus of 500 mL 5% albumin and starting dose of norepinephrine 0.1 mcg/kg/min, resulting in improvement of hemodynamics (BP increased to 92/63 mmHg, CVP reduced to 15 mmHg) and blood gas analysis (pH 7.37, pCO2 33 mmHg, pO2 123 mmHg, SaO2 99%). Gradual weaning of NO therapy was performed until postoperative day (POD) 2, but the patient experienced similar recurrent symptoms. Bedside echocardiography showed a D-shaped left ventricle (LV) and second grade LV diastolic dysfunction [5]. Furthermore, there was right-to-left shunt across the PFO with tricuspid valve gradient of 54 mmHg (Figs. 5A and 5B). No pulmonary regurgitation was observed, and the postoperative right ventricular outflow tract (RVOT) gradient persisted at 16 mmHg. No obstructed flow was seen between the repaired common pulmonary chamber and the left atrium. All these findings confirmed the diagnosis of pulmonary hypertension crisis in a relieved RVOT.
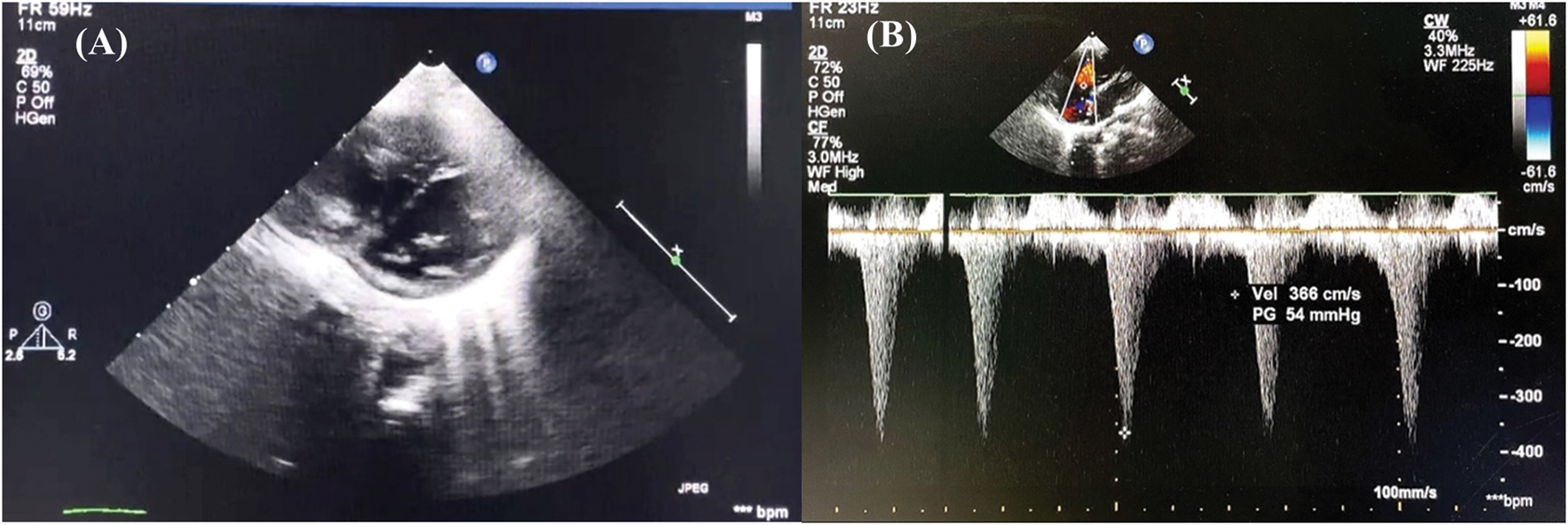
Figure 5: Postoperative day 2 echocardiography in intensive care unit demonstrates (A) left ventricle D-shaped with (B) tricuspid valve gradient 54 mmHg
20 ppm of NO was readministered followed by each 30 μg bolus of vecuronium and fentanyl. Anesthesia was maintained via combination of 5 μg/kg/hr of fentanyl, 0.1 mg/kg/hr of midazolam, and 0.1 mg/kg/hr of vecuronium. During monitoring, the patient’s BP increased to 82/65 mmHg, pO2 increased to 97 mmHg, and CVP reduced to 14 mmHg. We started treatment of sildenafil with an incremental dose increase over the next few days, indicated for pulmonary hypertension. On POD 10, echocardiography indicated a marked reduction of right ventricular (RV) pressure and left-to-right shunting across PFO along with tapering off the NO. The patient showed improvement in hemodynamic parameters, end-organ biomarkers, and blood gas analysis, who was transferred into the ward on POD 14. Eventually, the patient was discharged from the hospital on POD 20 with no sequelae.
Pulmonary hypertension crisis is characterized by hypotension, severely decreased saturation of oxygen, blood acidosis, and echocardiographic findings comprising a leftward deviation of the interventricular septum and development of interatrial right-to-left shunt [6,7]. During the operation, the surgeons used a valve-sparing technique to improve pulmonary blood flow through the stenosed RVOT. Increased right ventricular (RV) systolic pressure (seen as a D-shaped LV structure during echocardiography) in this patient was not predominantly due to RVOT obstruction, proven by the significant reduction of RVOT pressure gradient down to 16 mmHg after the operation. Additionally, the evidence of pre-existing pulmonary hypoplasia, as one of the main causes of increased RV systolic pressure after septal closure in TOF, was also not found in this patient [8].
The incidence of postoperative pulmonary hypertension crisis in patients with TAPVC varied depending on a certain population [9]. Meanwhile, in patients with TOF, pulmonary hypertension is an uncommon consequence following surgical repair with a prevalence of about 1% [10,11]. Postoperative RV dysfunction in TOF patients due to right ventricular outflow tract (RVOT) obstruction and right ventricle hypertrophy (RVH) could be exacerbated by suboptimal myocardial protection during surgery, long cardiopulmonary bypass time, and reperfusion lung injury [12–14]. Late repair surgery, in this patient, may result in less improved postoperative RV function, for it should be performed around the age of 3–12 months [15,16]. This condition may have generated less flow into the pulmonary artery and thus lowered the possible complication of pulmonary hypertension.
Despite the low pulmonary blood flow, pulmonary hypertension may happen due to the relatively non-compliant LV and small LA in patients with TAPVC [17]. In this case, there was a second-grade LV diastolic dysfunction found during postoperative echocardiographic assessment, which may confer a higher risk of developing pulmonary hypertension [18]. Failing left ventricle was associated with increased intraventricular pressure, which gives backward pressures to the previous connecting structures, such as the left atrium and pulmonary capillary beds. Along with the improved blood flow across RVOT after the operation, pressure could build up in the lung vasculatures, subsequently inducing a pulmonary hypertension crisis.
Discovery of MAPCAs during operation, as in this case, also becomes one of the rationales for the development of postoperative pulmonary hypertension related to TOF [10,19]. Their presence compensates for the lack of direct pulmonary blood flow, thus acting as an additional or primary source of blood supply to the lungs in patients with cyanotic congenital heart disease (CHD) [19,20]. Other multiple factors also contribute to pulmonary hypertension in patients with TOF and MAPCAs. Hypoplasia of pulmonary arterial beds due to reduced pulmonary blood flow, peripheral pulmonary stenosis, and vascular spasm in areas of alveolar hypoventilation were pathological characteristics reported in TOF with MAPCAs, which can potentially result in pulmonary vasculature remodeling. Evidence of medial hypertrophy, fibrous intimal proliferation, internal elastic lamina rupture, and plexiform lesions, similar to pulmonary vascular remodeling in pulmonary hypertension, have been found in MAPCAs through histologic examinations. These findings indicate that patients with TOF with MAPCAs may potentially encounter pulmonary hypertension after the operation [10].
In this report, the diagnosis could only be established after the patient experienced recurrent symptoms following termination of NO and was firmly examined by echocardiography. Since NO was recommended by the 2004 European Guidelines for the standard treatment and prevention of postoperative pulmonary hypertension, we were able to successfully manage the condition [21,22]. A dose of NO inhalation ranging between 5 to 80 ppm causes selective pulmonary vasodilation by triggering cyclic guanosine monophosphate (cGMP)-dependent signaling pathways in the pulmonary vascular smooth muscle cells [23,24]. We administered NO starting at 20 ppm, which rendered no adverse effects. The effectiveness of NO can be increased through careful patient selection, the use of additional drugs (in this case, sildenafil), and progressive withdrawal to prevent the risk of rebound pulmonary hypertension [25,26]. Sildenafil has also been demonstrated to increase arterial oxygenation in patients with pulmonary hypertension, thus eliciting beneficial hemodynamic responses. Evidence suggests that sildenafil is an effective supplementary therapy during the weaning off inhaled and intravenous NO [23]. The combination of NO with oral sildenafil has been shown to be safe and effective since it targets more therapeutic pathways with synergistic effects on the pulmonary vasculature. Oral sildenafil could also prevent rebound pulmonary hypertension following NO withdrawal while increasing the vasodilatory effects of NO [27].
This case is exceptional for a number of reasons. Postoperative pulmonary hypertension was diagnosed after observation of recurrent symptoms when stopping NO inhalation. The linked MAPCAs add further interest to this case report as it explains the possibility of pulmonary vessel remodeling, which accounts for precapillary pulmonary hypertension. Furthermore, postcapillary pulmonary hypertension could not be excluded, for there was a finding of LV diastolic dysfunction during echocardiography. The mechanism of the inhaled NO in postcapillary pulmonary hypertension could worsen left heart failure has not been well understood; on the other hand, improvement of symptoms after inhaling NO did not exclude the diagnosis of postcapillary pulmonary hypertension [28].
There are some limitations in terms of case management. Early primary repair, ideally, is not a frequent practice due to a variety of reasons, such as delayed diagnosis, financial constraints, and relatively poorer outcomes. Preoperative cardiac catheterization should be performed as a standard procedure to precisely characterize the heart anatomy although echocardiography can also diagnose the majority of these cases. Lastly, careful identification of MAPCAs in the CT scan would have resulted in the recommendation of pre-operative transcatheter closure if they were sizable and significant, yet it was missed during the imaging.
To conclude, patients with a combination of TOF and TAPVC could be at particular risk of developing postoperative pulmonary hypertension crisis, especially in the presence of MAPCAs, which potentially cause pulmonary vascular remodeling and finding of LV diastolic dysfunction. A successful outcome calls for meticulous preoperative workups and analyses of different kinds of perioperative anatomical lesions, as well as careful postoperative bedside care monitoring.
Acknowledgement: Authors would especially like to thank Gadjah Mada University and National Cardiovascular Center Harapan Kita who has provided extensive support.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: The authors confirm contribution to the paper as follows: Conception and design of the study, data analysis, data collection, and the creation of the manuscript draft: Kesumarini, D. Data collection and data analysis: Widyastuti, Y. Conceptualize the study design and data collection: Boom, C. E. and Dinarti, L. K. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials: Datasets generated during the current study available upon reasonable request.
Ethics Approval: The report was conducted in accordance with the Nuremberg Code and Declaration of Helsinki, and the protocol was approved by the Institutional Review Board of National Cardiovascular Center Harapan Kita (No. LB.02.01/VII/037/KEP037/2022). The guardians of the patient gave their informed consent for publication of patient’s information.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Talwar, S., Sandeep, J. A., Choudhary, S. K., Gulati, G. S., Airan, B. (2009). Tetralogy of Fallot with anomalous systemic and pulmonary venous drainage, anomalous coronary artery pattern, and abnormal development of diaphragm. Congenital Heart Disease, 4(1), 21–24 [Google Scholar]
2. Andropoulos, D. B., Stayer, S., Mossad, E. B., Miller-Hance, W. C. (2015). Anesthesia for congenital heart disease, 3rd editionUSA: John Wiley & Sons. [Google Scholar]
3. Gagnier, J. J., Kienle, G., Altman, D. G., Moher, D., Sox, H. et al. (2013). The CARE guidelines: Consensus-based clinical case reporting guideline development. British Medical Journal Case Report, 2(5), 38–43. [Google Scholar]
4. Cantinotti, M., Scalese, M., Murzi, B., Assanta, N., Spadoni, I. et al. (2013). Echocardiographic nomograms for ventricular, valvular, and arterial dimensions in caucasian children with a special focus on neonates, infants, and toddlers. Journal of the American Society of Echocardiography, 27(2), 179–191 [Google Scholar] [PubMed]
5. Porter, T. R., Shillcut, S. K., Adams, M. S., Desjardins, G., Glas, K. E. et al. (2015). Guidelines for the use of echocardiography as a monitor for therapeutic intervention in adults: A report from the American Society of Echocardiography. Journal of the American Society of Echocardiography, 28, 40–46 [Google Scholar] [PubMed]
6. Hung, D. Q., Huy, D. X., Vo, H. L., Hien, N. S. (2021). Factors associated with early postoperative results of total anomalous pulmonary venous connection repair: Findings from retrospective single-institution data in Vietnam. Integrated Blood Pressure Control, 14, 77–86 [Google Scholar] [PubMed]
7. Öztürk, E., Tanıdır, I. C., Ayyıldız, P., Kıplapınar, N., Özyılmaz, I. et al. (2015). Surgery-related complications and their management in total anomalous pulmonary venous return during intensive care unit stay. Turkish Journal of Thoracic and Cardiovascular Surgery, 23(2), 229–238. [Google Scholar]
8. Bhattacharya, S., Sen, S., Levy, P. T., Rios, D. R. (2019). Comprehensive evaluation of right heart performance and pulmonary hemodynamics in neonatal pulmonary hypertension. Current Treatment Options in Cardiovascular Medicine, 21(2), 10 [Google Scholar] [PubMed]
9. Prys-Roberts, C. (1984). Anaesthesia and hypertension. British Journal of Anaesthesia, 56(7), 711–724. [Google Scholar]
10. Yasuhara, J., Yamagishi, H. (2015). Pulmonary arterial hypertension associated with tetralogy of Fallot. International Heart Journal, 56, S17–S21 [Google Scholar] [PubMed]
11. Lindberg, L., Olsson, A. K., Jögi, P., Jonmarker, C. (2002). How common is severe pulmonary hypertension after pediatric cardiac surgery. Journal of Thoracic and Cardiovascular Surgery, 123(6), 1155–1163 [Google Scholar] [PubMed]
12. Levy, D., Laghlam, D., Estagnasie, P., Brusset, A., Squara, P. et al. (2021). Post-operative right ventricular failure after cardiac surgery: A cohort study. Frontiers in Cardiovascular Medicine, 8(6), 1–7. [Google Scholar]
13. Younis, M. M. K., Akhtar, S., Mohsin, M., Ahmad, W., Arshad, A. et al. (2019). Short and midterm outcome of fallot’s tetralogy repair in infancy: A single center experience in a developing country. Journal of Ayub Medical College Abbottabad, 31(3), 383–387. [Google Scholar]
14. Egbe, A., Mittnacht, A., Nguyen, K., Joashi, U. (2014). Risk factors for morbidity in infants undergoing tetralogy of Fallot repair. Annals of Pediatric Cardiology, 7(1), 13–18 [Google Scholar] [PubMed]
15. Tinmaswala, M. A., Saple, P. P., Gupta, A., Prachi, N., Nitinkumar, A. et al. (2015). Isolated major aortopulmonary collateral artery causing CCF in a newborn: A case report. International Journal of Medical Research & Health Sciences, 4(2), 471. [Google Scholar]
16. Mathew, R., Thilenius, O. G., Replogle, R. L., Arcilla, R. A. (1977). Cardiac function in total anomalous pulmonary venous return before and after surgery. Circulation, 55(2), 361–377 [Google Scholar] [PubMed]
17. Perez, V. A., Haddad, F., Zamanian, R. T. (2012). Diagnosis and management of pulmonary hypertension associated with left ventricular diastolic dysfunction. Pulmonary Circulation, 2(2), 163–169 [Google Scholar] [PubMed]
18. Patra, S., Srinivas, S. K., Agrawal, N., Jayaranganath, M. (2013). Isolated major aortopulmonary collateral artery in an infant presenting with recurrent lower respiratory tract infection. British Medical Journal Case Report, 2013, 2–3. https://doi.org/10.1136/bcr-2013-200421 [Google Scholar] [PubMed] [CrossRef]
19. Macrae, D. J., Field, D., Mercier, J. C., Møller, J., Stiris, T. et al. (2004). Inhaled nitric oxide therapy in neonates and children: Reaching a European consensus. Intensive Care Medicine, 30(3), 372–380 [Google Scholar] [PubMed]
20. Germann, P., Braschi, A., Rocca, G. D., Dinh-Xuan, A. T., Konrad, F. et al. (2005). Inhaled nitric oxide therapy in adults: European expert recommendations. Intensive Care Medicine, 31(8), 1029–1041 [Google Scholar] [PubMed]
21. Brunner, N., de Jesus Perez, V. A., Richter, A., Haddad, F., Denault, A. et al. (2014). Perioperative pharmacological management of pulmonary hypertensive crisis during congenital heart surgery. Pulmonary Circulation, 4(1), 10–24 [Google Scholar] [PubMed]
22. Khanna, S., Choudhury, M., Kiran, U. (2009). Total anomalous pulmonary venous connection: Post operative problems and management. Indian Journal of Anesthesiology, 53(1), 71–74. [Google Scholar]
23. Namachivayam, P., Theilen, U., Butt, W. W., Cooper, S. M., Penny, D. J. et al. (2006). Sildenafil prevents rebound pulmonary hypertension after withdrawal of nitric oxide in children. American Journal of Respiratory and Critical Care Medicine, 174(9), 1042–1047 [Google Scholar] [PubMed]
24. Mossad, E. B. (2001). Pro: Intraoperative use of nitric oxide for treatment of pulmonary hypertension in patients with congenital heart disease is effective. Journal of Cardiothoracic and Vascular Anesthesia, 15(2), 259–262 [Google Scholar] [PubMed]
25. Matamis, D., Pampori, S., Papathanasiou, A., Papakonstantinou, P., Tsagourias, M. et al. (2012). Inhaled no and sildenafil combination in cardiac surgery patients with out-of-proportion pulmonary hypertension acute effects on postoperative gas exchange and hemodynamics. Circulation Heart Failure, 5(1), 47–53 [Google Scholar] [PubMed]
26. Atz, A. M., Lefler, A. K., Fairbrother, D. L., Uber, W. E., Bradley, S. M. (2002). Sildenafil augments the effect of inhaled nitric oxide for postoperative pulmonary hypertensive crises. Journal of Thoracic and Cardiovascular Surgery, 124(3), 628–629 [Google Scholar] [PubMed]
27. Stocker, C., Penny, D. J., Brizard, C. P., Cochrane, A. D., Soto, R. et al. (2003). Intravenous sildenafil and inhaled nitric oxide: A randomised trial in infants after cardiac surgery. Intensive Care Medicine, 29(11), 1996–2003 [Google Scholar] [PubMed]
28. Naeije, R., Chin, K. (2019). Differentiating precapillary from postcapillary pulmonary hypertension. Circulation, 140, 712–714 [Google Scholar] [PubMed]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools