 Open Access
Open Access
CASE REPORT
Primary renal aspergilloma: a challenge to endure—a case report
1 Karnataka Medical College and Research Institute, Rajiv Gandhi University of Health Sciences, Hubli, 580022, India
2 KIMS-SUNSHINE, Sunshine Hospital, Begumpet, Hyderabad, 5000016, India
3 Krishna Vishwa Vidyapeeth, Krishna Institute of Medical Science, Karad, 415539, India
* Corresponding Author: Sarbjit Mohapatra. Email:
Canadian Journal of Urology 2025, 32(5), 509-513. https://doi.org/10.32604/cju.2025.063783
Received 23 January 2025; Accepted 11 June 2025; Issue published 30 October 2025
Abstract
Background: Isolated renal aspergilloma is a rare medical entity posing difficult diagnostic and treatment challenges. Case Description: We document a case of Primary Renal Aspergilloma in a 55-year-old male with diabetes mellitus, hypertension, and chronic liver disease. The individual presented with features of obstructive uropathy due to fungal balls requiring retrograde endoscopic intervention and drainage. The cheesy material retrieved during the procedure was identified as an Aspergilloma on histopathology. Due to far and fewer reports in the medical literature, there have been no standard diagnostic & management strategies, which in turn has resulted in unacceptably high mortality. Conclusion: Isolated renal aspergilloma is an uncommon medical condition with intricate diagnostic and treatment pathways. Due to the rarity of the disease, there is no established protocol for the treatment of renal aspergillomas. Further research is necessary to improve diagnostics, optimize treatments, and enhance clinician awareness for early detection and management.Keywords
Aspergillosis is an opportunistic fungal infection with numerous species that primarily affects the lungs, though in rare cases, other organs, including the kidneys. Renal Aspergilloma is very rare, with only 100 cases reported in medical literature ever since Dr. Ross first described the condition, as Nephromycosis Aspergillina in 1891.1,2 Renal aspergillosis in immunocompromised patients can result in potentially life-threatening conditions carrying high mortality rates.3 Because of its non-specific presentation, it affords significant clinical challenges. With the rising incidence of risk factors like Diabetes, chronic liver diseases, chronic steroid use, prolonged antibiotics therapy, and invasive intervention, renal aspergilloma is being increasingly seen, even in immunocompetent patients.4
This study was approved by the institutional ethics committee. The handwritten informed consent was obtained from the patient. This case report was written following the CARE guidelines and the accompanying checklist.5
A 55-year-old male presented to Karnataka Medical College and Research Institute with intermittent left flank pain of 6 months duration and passing grey to white material in the urine. He had been on regular treatment for diabetes mellitus, hypertension, and chronic liver disease for 1 year (Figure 1). There was neither any history of chronic steroid usage nor any history of any Sodium Glucose Transport-2 (SGLT-2) inhibitors for his Diabetes. There was no previous record of catheterization or any interventions.
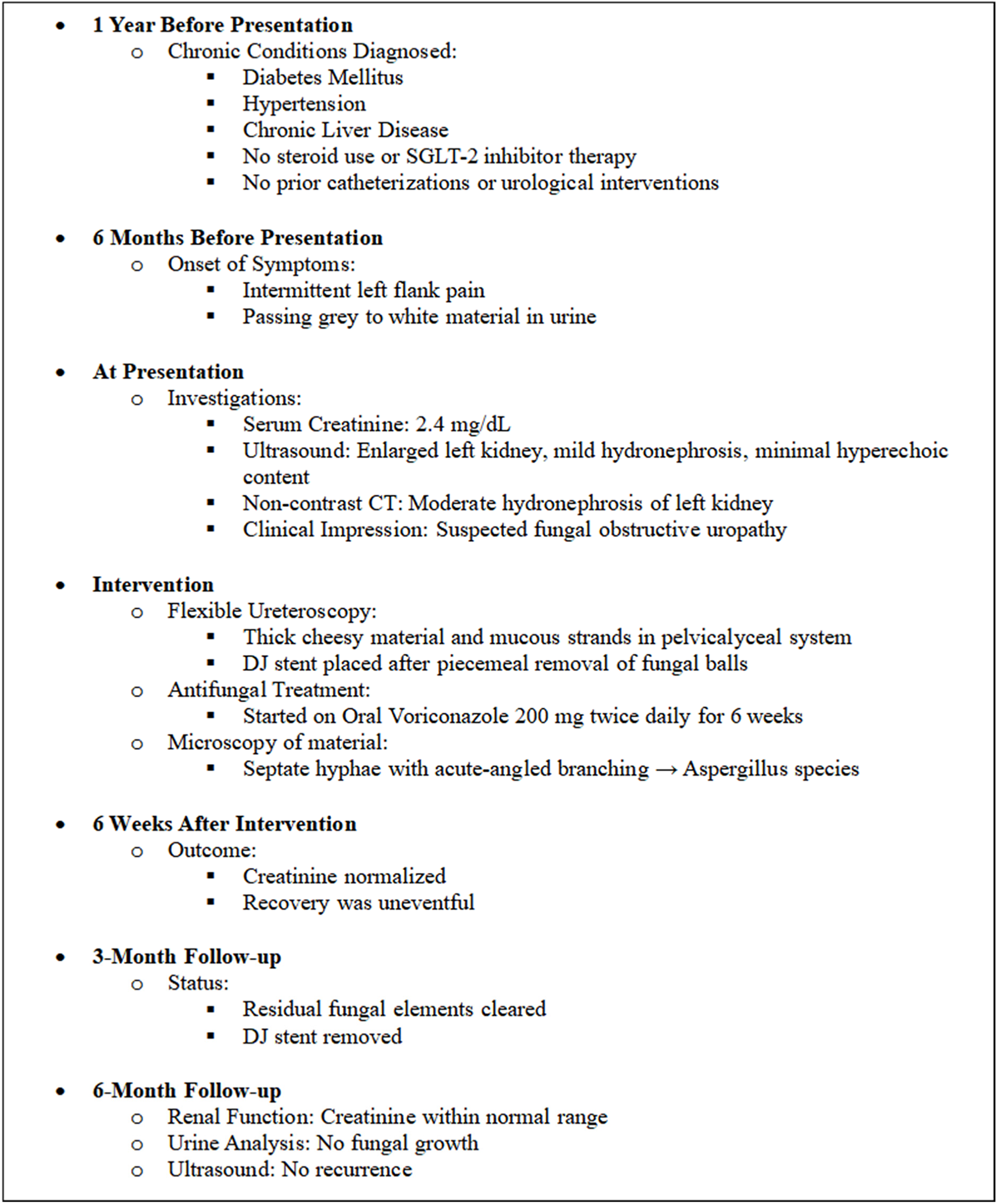
FIGURE 1. Timeline of the case scenario
On investigations, the renal function was mildly deranged with creatinine of 2.4 mg/dl, enlarged left kidney with minimal hyperechoic content mild hydronephrosis on ultrasound examination. Further imaging with a non-contrast computed tomography scan showed a moderately hydronephrotic left kidney (Figure 2). Given persistent raised creatinine and features of obstructive uropathy intervention with a flexible ureteroscope was done, which showed thick cheesy material with mucous strands within the pelvi-calyceal system (Figure 3). A double J (DJ) stent was placed after clearing most fungal balls piecemeal. Oral Voriconazole 200 mg twice daily was started and continued for 6 weeks. The recovery was uneventful with creatinine returning to normal levels. The retrieved material, on microscopy, showed large colonies of septate hyphal forms with parallel walls and slender acute-angled branching, consistent with Aspergillus species (Figure 3).
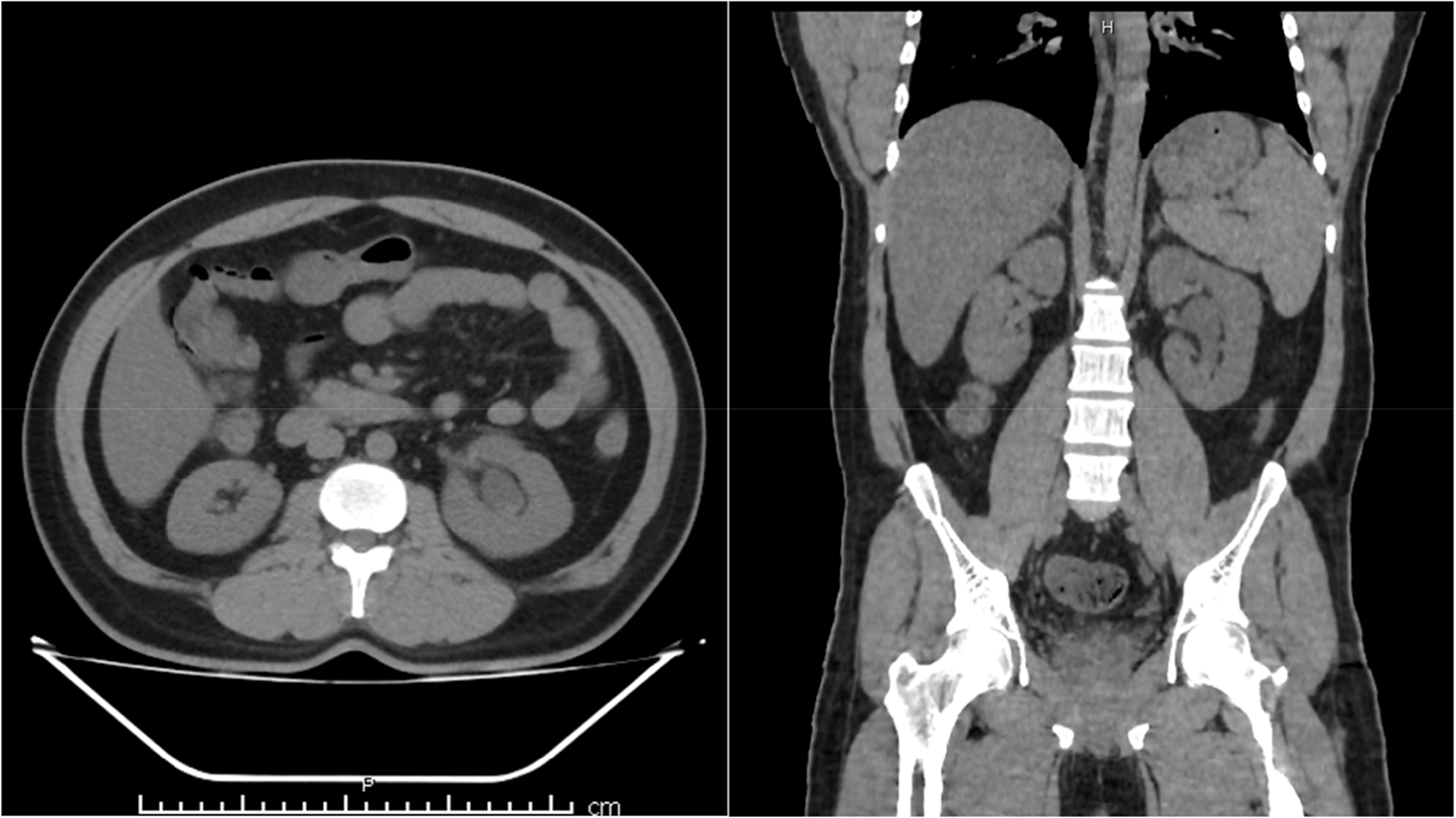
FIGURE 2. Axial and coronal cut section showing left hydronephrotic kidney
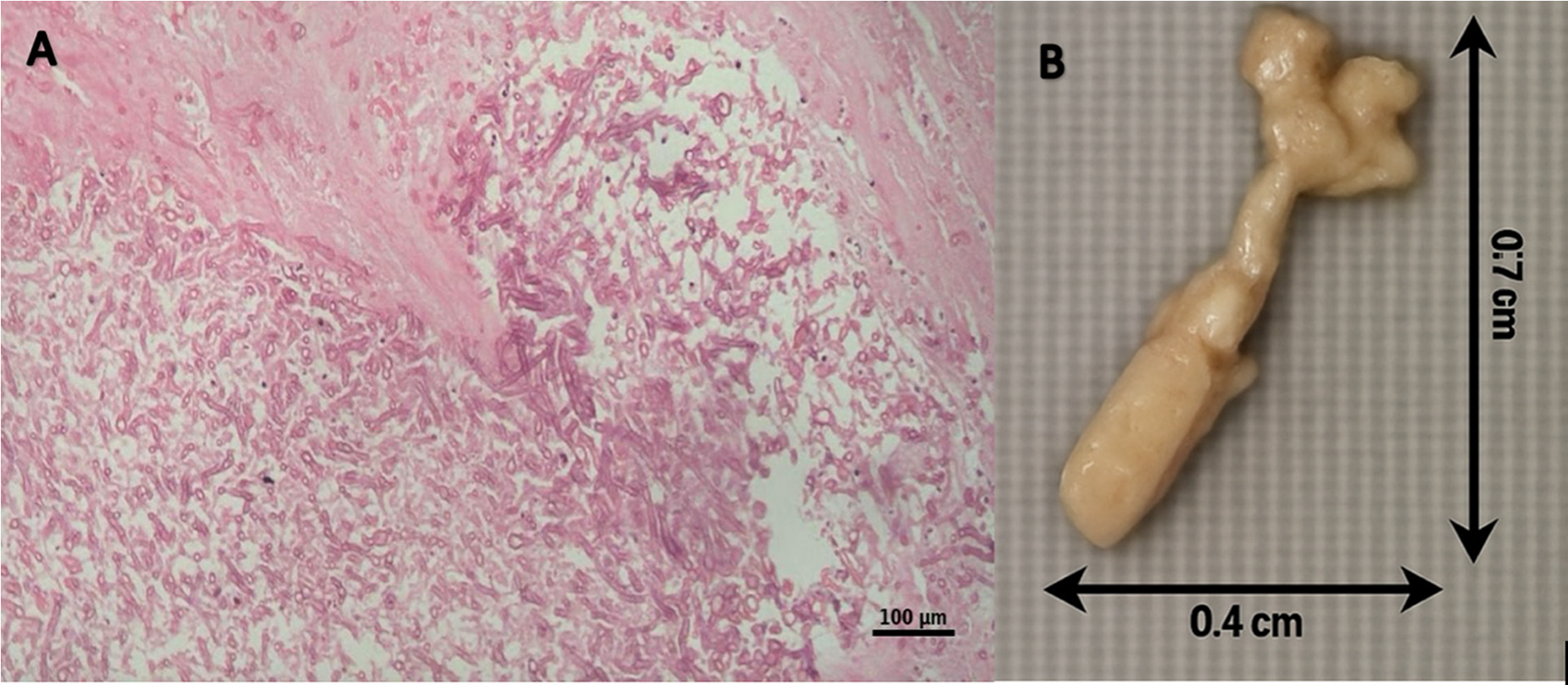
FIGURE 3. Microscopic and macroscopic images. A. Hematoxylin and eosin-stained histological section showing large colonies of septate hyphal forms of fungi with parallel walls and slender acute-angled branching (high magnification 100× power field). B. Fungal ball piece meal measuring 0.7 × 0.4 cm removed during retrograde intrarenal surgery (RIRS) procedure
At 3 months of follow-up, residual fungal elements were cleared, and the stent was removed. Further, in follow-up at 6 months patient’s serum creatinine was within normal range. Urine analysis, along with fungal culture, was negative and ultrasound did not show any recurrence.
Historically, A fumigatus is recognised as the primary pathogen amongst the Aspergillus family because of its ability to thrive in a wide range of environmental conditions and enhanced virulence factors.6 Aspergillii are commensals in the human host and an alteration in the host immunologic defense mechanism enhances host susceptibility and the invading potential of fungal elements to cause invasive and serious diseases.7,8 Involvement in the genitourinary system could be attributed either to hematogenous spread or to ascending infection. There are three primary modes in which the infection may be transmitted: hematogenous dissemination, which is more prevalent in immunocompromised patients; direct inoculation after trauma or surgery; and ascending spread which is frequently associated with indwelling bladder catheters.1,9,10 Primary renal aspergillosis as a clinical entity has rarely been described mainly in patients with immunocompromised states such as HIV infection, malignancy (especially myeloproliferative or lymphoproliferative disorders), renal transplant recipients on immunosuppression, and patients receiving chemotherapy and radiation.11,12 Other significant risk factors include diabetes mellitus, collagen vascular disease, sarcoidosis, chronic use of steroids, prior urological intervention, and prolonged antibiotic use. Patients receiving SGLT-2 inhibitors have a higher preponderance for urinary fungal infections because of their ability to induce glycosuria and hence provide a conducive environment for fungal growth.1,6,13
The primary symptoms in reported cases are prolonged fever and a reduction in the glomerular filtration rate. Radiological imaging methods such as ultrasonography or computed tomography are crucial to identify associated genitourinary tract abnormalities or renal abscess formation. Urine culture for Aspergillus has low sensitivity and is positive in only 25% of the cases.6,14,15 The patient being reported passed cheesy material in urine often mentioned as “white clots” and confused with necrotic papillae. Histopathological studies are confirmatory in the diagnosis of renal aspergilloma being the primary diagnostic method in over 70% of the reported cases.16 Recent studies have shown that radioisotopes Strontium 85 may be used to localize Aspergillus infection and that the use of novel biomarkers has diagnostic potential.17
The rarity of the disease not only poses significant diagnostic challenges but also lacks a protocol for the optimal treatment of renal aspergillomas.18 In the studies by Bongomin, unacceptably high mortality of 28% highlights the need for an optimal treatment approach depending on factors such as the extent of renal involvement, and the presence of complications.1,19 Anti-mycotic drug resistance reported for Aspergillus fumigatus infections adds to therapeutic challenges and leads to aggressive disease manifestations. The guidelines of the Infectious Diseases Society of America for the treatment of aspergillosis suggest a comprehensive approach, including both medical and urologic strategies while treating renal aspergillosis.2,3 Relief of ureteral obstruction with local instillation of amphotericin B deoxycholate through a nephrostomy tube is often the mainstay of treatment strategy in luminal infections. The flexible ureteroscopes provide better visualization of the upper urinary tract and may aid in retrograde drainage of debris followed by the instillation of amphotericin. Although it can avoid any transcutaneous intervention and further complications, however, ureteroscopic intervention is known to cause increased intrarenal pressure leading to a serious risk of sepsis. For parenchymal disease, Voriconazole is the preferred treatment. Medical management is recommended for smaller abscesses, and surgical drainage is indicated for larger abscesses. Microwave ablation has demonstrated potential as an alternate therapy in certain instances when surgery is not an option. Nephrectomy is often a last resort when medical therapy has failed.9,16
Maintaining a high index of suspicion and early administration of antifungals are crucial for better outcomes. Further research is necessary to develop standardized treatment plans and investigate cutting-edge therapeutic approaches to enhance patient outcomes and reduce mortality to acceptable levels.
Acknowledgement
Not applicable.
Funding Statement
The authors received no specific funding for this study.
Author Contributions
The authors confirm contribution to the paper as follows: conceptualization, design, supervision: Nandkumar Madhekar; formal analysis, definition of intellectual content, manuscript review: Jaideep Ratkal; literature search, image editing: Sameer Ratkal; data search, writing—original draft preparation, review and editing: Sarbjit Mohapatra. All authors reviewed the results and approved the final version of the manuscript.
Availability of Data and Materials
Not applicable.
Ethics Approval
Karnataka Medical College and Research Institute, Hubballi Ethics Committee [Reg No.: ECR/486/Inst/KA/2013/RR-20] held on 26th November 2024 has approved the study title: Primary Renal Aspergilloma: A Challenge to Endure by Dr. Sarbjit Mohapatra.
Informed Consent
For this case report, informed consent was performed and patient signed consent form to carry out this case report. Evidence is available for review by editor upon request.
Conflicts of Interest
The authors declare no conflicts of interest to report regarding the present study.
References
1. Bongomin F, Morgan B, Ekeng BE et al. Isolated renal and urinary tract aspergillosis: a systematic review. Ther Adv Urol 2023;15:1–18. doi:10.1177/17562872231218621. [Google Scholar] [PubMed] [CrossRef]
2. Al-Ibraheem H, Shaker G, Roushias S. Isolated renal aspergilloma. Urol Case Rep 2024;53(4):102688. doi:10.1016/J.EUCR.2024.102688. [Google Scholar] [PubMed] [CrossRef]
3. Patterson TF, Thompson GRIII, Denning DW et al. Practice guidelines for the diagnosis and management of aspergillosis: 2016 update by the infectious diseases society of America. Clin Infect Dis 2016;63(4):e1. doi:10.1093/CID/CIW326. [Google Scholar] [PubMed] [CrossRef]
4. Ray A, Adarsh Aayilliath K, Banerjee S, Chakrabarti A, Denning DW. Burden of serious fungal infections in india. Open Forum Infect Dis 2022;9(12):1–10. doi:10.1093/ofid/ofac603. [Google Scholar] [PubMed] [CrossRef]
5. Riley DS, Barber MS, Kienle GS et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol 2017;89(7216):218–235. doi:10.1016/j.jclinepi.2017.04.026. [Google Scholar] [PubMed] [CrossRef]
6. Warshawsky AB, Keiller D, Gittes RF. Bilateral renal aspergillosis. J Urol 1975;113(1):8–11. doi:10.1016/S0022-5347(17)59393-3. [Google Scholar] [PubMed] [CrossRef]
7. Irby PB, Stoller ML, McAninch JW. Fungal bezoars of the upper urinary tract. J Urol 1990;143(3):447–451. doi:10.1016/s0022-5347(17)39987-1. [Google Scholar] [PubMed] [CrossRef]
8. Sud K, D’cruz S, Kohli HS et al. Isolated bilateral renal aspergillosis: an unusual presentation in an immunoeompetent host. Ren Fail 1998;20(6):839–843. doi:10.3109/08860229809045181. [Google Scholar] [PubMed] [CrossRef]
9. Cadena J, Thompson GR3rd, Patterson TF. Aspergillosis: epidemiology, diagnosis, and treatment. Infect Dis Clin North Am 2021;35(2):415–434. doi:10.1016/j.idc.2021.03.008. [Google Scholar] [PubMed] [CrossRef]
10. Flechner SM, McAninch JW. Aspergillosis of urinary tract: ascending route of infection and evolving patterns of disease. J Urol 1981;125(4):598–601. [Google Scholar] [PubMed]
11. Salgia P, Mani MK. Renal aspergillosis-case report. Nephron 1985;40(3):376–378. doi:10.1159/000183498. [Google Scholar] [PubMed] [CrossRef]
12. Martinez-Jabaloyas J, Osca JM, Ruiz JL, Beamud A, Blanes M, Jimenez-Cruz JF. Renal aspergillosis and AIDS. Eur Urol 1995;27(2):167–169. [Google Scholar] [PubMed]
13. Maquera-Afaray J, Luna-Vilchez M, Portillo-Alvarez D, López JW. Primary renal aspergillosis in a newborn: a case report and review of the literature on children. Turkish J Pediatrics 2022;64(3):580–584. doi:10.24953/turkjped.2021.796. [Google Scholar] [PubMed] [CrossRef]
14. Bubler M. Acute ureteral colic from an obstructing renal aspergilloma. Rev Infect Dis 1987;9(4):790–794. [Google Scholar]
15. Krishnamurthy R, Aparajitha C, Abraham G, Shroff S, Sekar U, Kuruvilla S. Renal aspergillosis giving rise to obstructive uropathy and recurrent anuric renal failure. Geriatr Nephrol Urol 1998;8(3):137–139. doi:10.1023/A:1008343315440/METRICS. [Google Scholar] [CrossRef]
16. Latgé JP, Chamilos G. Aspergillus fumigatus and aspergillosis in 2019. Clin Microbiol Rev 2019;33(1):e00140-18. doi:10.1128/CMR.00140-18. [Google Scholar] [PubMed] [CrossRef]
17. Rawal BD, Adiseshan N. Mechanism of uptake of strontium isotopes in aspergillus lesions. Am Rev Respir Dis 1976;113(3):331–335. doi:10.1164/ARRD.1976.113.3.331. [Google Scholar] [PubMed] [CrossRef]
18. Hung YH, Lai HH, Lin HC, Sun KS, Chen CY. Investigating factors of false-positive results of aspergillus galactomannan assay: a case-control study in intensive care units. Front Pharmacol 2021;12:1–6. doi:10.3389/fphar.2021.747280. [Google Scholar] [PubMed] [CrossRef]
19. Duthie R, Denning DW. Aspergillus fungemia: report of two cases and review. Clin Infect Dis 1995;20(3):598–605. doi:10.1093/CLINIDS/20.3.598. [Google Scholar] [CrossRef]
Cite This Article
 Copyright © 2025 The Author(s). Published by Tech Science Press.
Copyright © 2025 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools