 Open Access
Open Access
ARTICLE
The Mediating Role of Religious Beliefs in the Relationship between Well-Being and Fear of the Pandemic
1
Faculty of Psychology, Ho Chi Minh City University of Education, Ho Chi Minh City, 700000, Vietnam
2
Faculty of Social Sciences and Public Relations, HUTECH University, Ho Chi Minh City, 700000, Vietnam
3
Department of Medical Services, Ministry of Public Health, Somdet Phra Sungharaj Nyanasumvara Geriatric Hospital, Chon Buri,
20150, Thailand
4
Department of Psychiatry, Faculty of Medicine, Chulalongkorn University, Bangkok, 10330, Thailand
* Corresponding Author: My-Tien Nguyen-Thi. Email:
(This article belongs to the Special Issue: Coping with Life Stress During/After the COVID-19 Pandemic and Its Impact on Mental Health)
International Journal of Mental Health Promotion 2023, 25(9), 1019-1031. https://doi.org/10.32604/ijmhp.2023.029235
Received 08 February 2023; Accepted 03 April 2023; Issue published 10 August 2023
Abstract
Religion is one of the social entities that has had a significant impact on the pandemic. The study’s goals are to investigate the relationship between well-being and fear of COVID-19, as well as to test whether religious beliefs mediate the effect of wellbeing on fear of COVID-19. The sample comprised of 433 participants in Vietnam. Independent Sample t-Test, One-way ANOVA, mediation analysis were used to analyze the data. In the levels of well-being, individuals who engage in religious services daily have higher levels than those hardly and never attend, and people from the age of 18 to 30 have higher levels than individuals from 31 to above 60 years. In addition, people aged from 51 to above 60 have higher levels of religious beliefs than people aged from 18 to 50. Females experience more fear of COVID-19 compared to males. The latter illustrates that religious beliefs mediate the effect of well-being on fear of COVID-19. Social workers and clinicians must prioritize older adults and people with chronic diseases for early mental interventions, and they should be aware of the role of religion in psychological treatment integration.Keywords
Before April 2021, Vietnam was one of just a handful of countries in the world to have avoided the COVID-19 pandemic [1]. However, more than a year after the first case was reported, Vietnam began its fourth pandemic wave [2]. On December 31, 2021, 1,728,405 confirmed cases and 39,133 deaths were documented during the continuing wave [3]. The country accounted for 99.6% and 99.9%, respectively, of total cases and deaths [2]. The pandemic has caused extraordinary social, including prolonged isolation, financial uncertainty, dramatic change in habits, and a fundamental adjustment to family life for billions of people around the globe [4,5]. The pandemic not only caused grave hazards to physical health, but also had detrimental effects on the population’s social, psychological, and mental health [6]. People experienced high levels of dread and worry due to the COVID-19 pandemic, which resulted in dramatic changes to their lifestyles, including their religious beliefs and behaviors [7].
Well-being and religious beliefs
Religiosity and spirituality should be studied as factors related to mental health during disasters [8–10], because religious beliefs play a significant role in people’s understanding of themselves and the world, as well as well-being [11]. People can draw on their beliefs and practices to find the meaning of confusing and painful moments [10]. Especially during the pandemic, individuals are likely to experience burnout due to the protracted, persistent stream of bad news and setbacks and a lack of improvement in their situation [12]. People who hold religious or spiritual views may have hope that things will change soon [13].
Religious beliefs and fear of COVID-19
Fear has been one of the most common psychological reactions in the general population during the pandemic [14,15]. Fear is an emotional response to a threat that is considered a functional, adaptive and transient response to stimuli causing physiological changes for a brief period [16,17]. Individuals with a higher threat perception are more likely to suffer negative consequences to their well-being. Threat perception in the pandemic is related to people’s perceptions of how the COVID-19 pandemic may cause unfavorable consequences. Individuals report feeling fearful of COVID-19 may threaten their mental health [18].
Religion has been considered to be a crucial coping tool when people are confronted with adversity [19,20]. Religion, prayer and other personal religious activities could be considered common strategies for religious believers dealing with the fear caused by COVID-19 [21]. During the pandemic, however, public restrictions were implemented, such as only going outside when an emergency, buying food or medicines and prohibiting large public gatherings, which led religious believers to refrain from gathering and participating in communal activities like worshipping, celebrating or Bible reading. Religious people felt the loss of engagement between fellowship and religious communities [22], compromised religious lifestyles and raised fear of COVID-19 [23] due to mandatory prohibitions against praying in a church.
Gender is one of the aspects that influences an individual’s health and disease status. Previous research indicated that females, as compared to males, were more susceptible to stress and, as a result, had higher levels of fear when confronted with various life events [24,25]. Besides, females reported that had a higher affective intensity and were more likely to experience negative emotions such as fear [26].
History of chronic disease and well-being
Prior studies have examined the relationship between well-being and individuals with chronic diseases. Prior evidence showed that people without chronic disease had much greater health and well-being than people with chronic disease [27]. Concerning the outbreak of COVID-19, a prior study found that individuals with chronic disease had greater levels of stress, anxiety, and depression [28], as well as lower psychological well-being and higher fears and worries about the COVID-19 [29] compared to individuals without the chronic disease.
Religious attendance and well-being
Many prior studies reported that religious attendance was linked to mental health enhancement, including decreased depressive symptoms, reduced anxiety and increased life satisfaction [30,31]. In addition, frequent religious attendance might have helped prevent the development of high levels of medical illness burden and better physical function [32]. Religious people feel sacredness to ordinary activities and receive spiritual comfort contributing to feelings of hope, optimism, peace and the release of negative emotions [33]. People’s religious beliefs are specifically strengthened by frequent participation in networks of people who share their beliefs. Graham et al. [34] reported that religious activities positively affected well-being among individuals, and the belief related to religion could be accounted for well-being. Besides, religious activities such as prayer, meditation, listening to religious radio programs or Bible reading had positive implications for the well-being of believers [35,36]. Many scholars reported a positive relationship between the frequency of religious service attendance and individuals’ well-being [11,22,37]. Individuals who regularly attend religious services may feel optimism, belonging, peacefulness, hope, and release of negative emotions [38,39].
The literature showed that the emotional experiences of older people were more steady, positive, and a greater sense of well-being than younger people [40,41]. According to Carstensen et al. [42], older people have more adaptation mechanisms to adversity, stress, and emotionally negative events than younger ones. Previous findings showed that older people had higher emotional well-being than younger people during the pandemic [43,44]. Older adults experienced lower stress from the pandemic, lower social isolation, less life change and less poor relationship quality than younger adults [45]. Older adults appeared to have higher resilience and systems for regulating their feelings and dealing effectively with adversity [46].
The most vulnerable age group to the pandemic has been identified as older individuals [47]. Religious beliefs and practices have been shown to assist people in managing stress and anxiety, and have been linked to less anxiety and more hope, particularly among older adults. Older adults had higher levels of religiosity than younger adults [48]. The elderly found that religious strategies help them manage loneliness, purpose and meaning of life, physical limitations and losses related to aging. It is also possible that older people have more free time to dedicate to religious contemplation and activity than younger people.
Vietnam is a multi-religious country where thousands of religious activities occur yearly [49]. In light of the pandemic, most people are considerably more open to faith, prayer, Bible reading, and worship. These religious activities give people control over the situation and deal with the fear of the pandemic. In the context of COVID-19, general public religious practices were considered unnecessary, and religious organizations were required not to organize mass activities. These restrictions influenced the general population’s mental health. Additionally, no research has studied the relationship between religious beliefs and well-being among the general population, particularly during the COVID-19 pandemic in Vietnam. For that reason, our research aims to investigate the association between well-being and fear of the pandemic, well-being and religious beliefs, and to determine if well-being and religious beliefs predict fear of the pandemic. Besides, we also examine the differences between demographic subgroups (age, gender, and chronic disease) in religious beliefs, well-being, and fear of the pandemic dimensions among the Vietnamese population.
Accordingly, the answers to the following questions were sought:
What factors influence the fear of COVID-19 in the general population?
Do religious beliefs act as a mediator between well-being and fear of COVID-19?
Literature was collected from Web of Science Core Collection and Scopus dataset over the period 1970–2022. The literature review was conducted in three steps: (1) exploring knowledge evolution, and knowledge frontiers; (2) content analysis; and (3) discussions, identifying future research directions. The collected information included titles, authors, subjects, publication years, keywords, abstracts, and cited references. This study used multiple terms referring to “fear of COVID-19”, “religious beliefs”, and “well-being” to carry out the literature search in the dataset. The data included papers (original research and review articles) and books. The search was conducted on October 15th, 2021. We identified over 80 initial sources from our search. Because the analysis of knowledge evolution and knowledge frontiers is typically based on historical research, the latest studies are relatively overlooked. To identify future research directions, we searched and analyzed studies published from 2015 to 2022.
Hypothesis 1: Females would be more likely to experience fear of COVID-19 than males.
Hypothesis 2: People without chronic disease would experience more well-being than people with chronic disease.
Hypothesis 3: Individuals who engage in religious services daily would experience more well-being than those who hardly and never attend.
Hypothesis 4: Older adults would experience more well-being than younger and middle adults.
Hypothesis 5: Older adults would have higher levels of religious beliefs than younger and middle adults.
Hypothesis 6: Religious beliefs negatively predict the fear of COVID-19 among the general population.
Hypothesis 7: Religious beliefs play a mediating role in the relationship between well-being and the fear of COVID-19.
Using the statistical formula for cross-sectional study design with a single proportion:
Sample Size =
Public restrictions were still implemented as prohibiting large public gatherings [51]. Thus, we used a Google Forms online survey through email and social media platforms to collect data from November 14th to December 31st, 2021 taking roughly 10–15 min to complete.
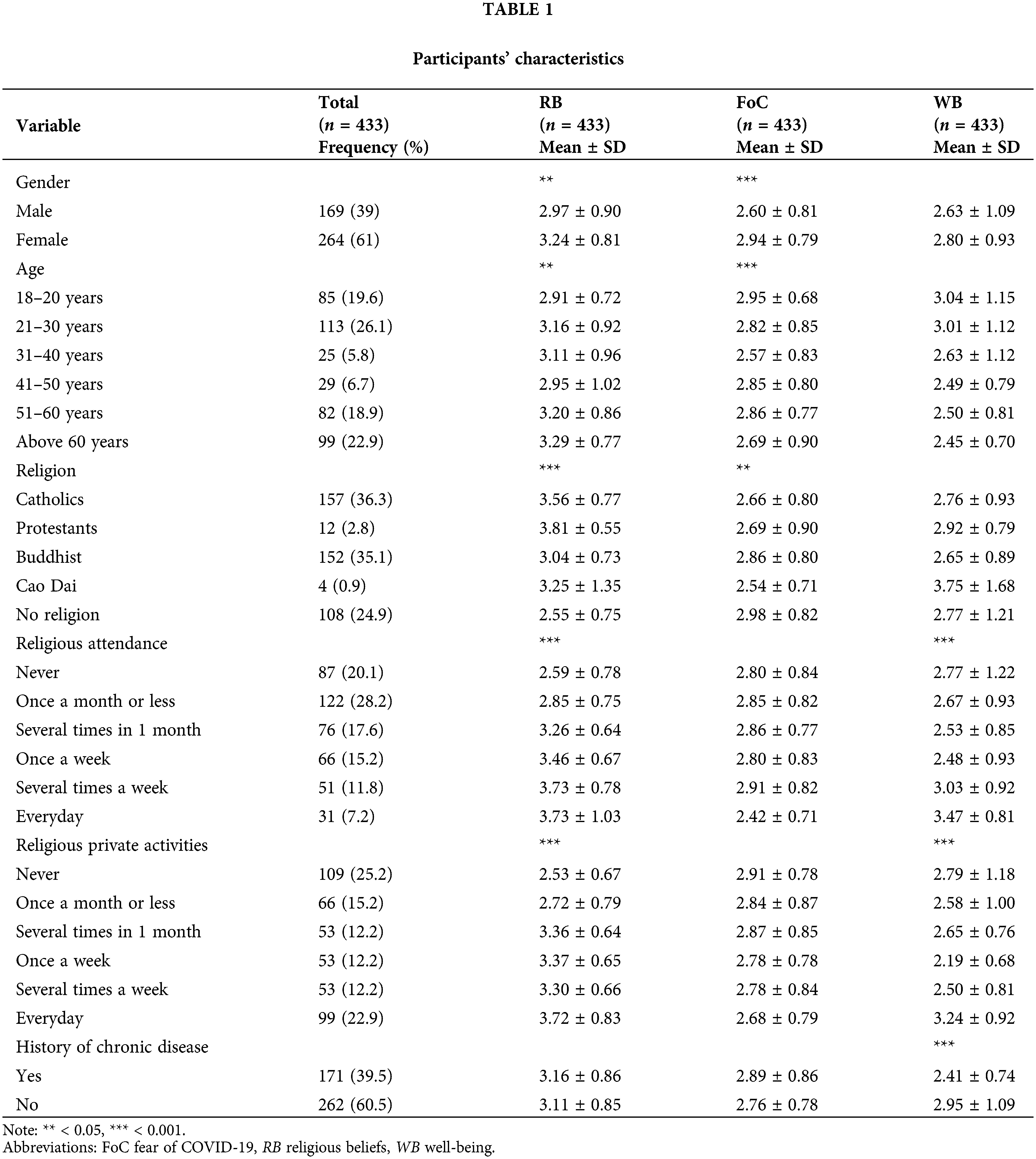
A total of 483 questionnaires were distributed, with 433 completed the survey providing a response rate of 89.65%, which is more than the 30% response rate most researchers demand in a study [52]. Among the participants (over 18 years), 169 (39%) were males and 264 (61%) were females. Participants’ ages ranged from 18–20 years (n = 85; 19.6%), 21–30 years (n = 113; 26.1%), 31–40 years (n = 25; 5.8%), 41–50 years (n = 29; 6.7%), 51–60 years (n = 82; 18.9%), and above 60 years (n = 99; 22.9%). In our study, younger adults aged from 18 to 30, middle adults aged from 31 to 50, and older adults aged from 51 and above 60. The participants’ religions were Catholicism (n = 157; 36.3%), Buddhism (n = 152; 35.1%), Protestantism (n = 12; 2.8%), Caodaism (n = 4; 0.9%), and non-religion (n = 108; 24.9%), most respondents did not have history of chronic disease (n = 262; 60.5%) as presented in Table 1.
Informed consent was provided before taking the survey, participation was voluntary without remuneration and respondents could withdraw at any time during data collection. Participants who had any questions were advised to email the research team. Participants were informed of the objectives of the study and asked to provide sociodemographic data including gender, age, religion, history of chronic disease, religious attendance and religious private activities.
The Intrinsic Religious Motivation Scale [49] was forward and back-translated into Vietnamese and English versions by two professional translators (a native speaker of Vietnamese who is fluent in English and vice versa). Eventually, the research team assessed for content, consistency and discrepancies between the original and the two translated versions.
The intrinsic religious motivation scale (IRMS)
The Intrinsic Religious Motivation Scale—10 items was developed by Hoge [49] to evaluate diverse approaches to religion and motivation through religious activities. Each item was responded to on a 5-point Likert scale ranging from 1 to 5 (strongly disagre to strongly agree) (e.g., “My religious beliefs are what really lie behind my whole approach to life”). The 10-item scale’s reliability was 0.901 [49].
In this study, Cronbach’s alpha for the overall scale was 0.874. The CFA indicated that the measurement was an adequate fit CMIN/df = 2.835 (p < 0.001); Goodness-of-fit index (GFI) = 0.973; Comparative fit index (CFI) = 0.981; Tucker–Lewis Index (TLI) = 0.972; Root means square error of approximation (RMSEA) = 0.065; and 90% Confidence Interval (CI: 0.042, 0.089) [53].
The fear of COVID-19 scale (FCV-19S)
The Fear of COVID-19 Scale—7 items was developed to measure individuals’ fear of COVID-19 [54]. Participants express their level of agreement using a 5-point Likert scale ranging from 1 to 5 (strongly disagre to strongly agree). This study utilized the Vietnamese version of the FCV-19S with a Cronbach’s alpha of 0.90 indicating a high level of internal consistency [55].
In this study, Cronbach’s alpha for the overall scale was 0.867. CMIN/df = 5.983 (p < 0.001); GFI = 0.960; CFI = 0.962; TLI = 0.920; RMSEA = 0.10; and 90% CI (0.082, 0.134) showing the measurement was an acceptable fit [53].
Mental health continuum–short form (MHC-SF)
The Mental Health Continuum Scale–Short Form with 14-item was developed by Keyes et al. [56] focusing on dimensions of well-being to assess happiness levels among individuals with 6-point Likert scale from 0 to 5 (never to everyday). The Vietnamese version of MHC-SF with a Cronbach’s alpha of 0.73 on the adult sample was used in this investigation [57].
In this study, Cronbach’s alpha for the overall scale was 0.929. CMIN/df = 3.842 (p < 0.001); GFI = 0.916; CFI = 0.942; TLI = 0.929; RMSEA = 0.081 and 90% CI (0.071, 0.091) showing the measurement was an adequate fit [53].
Initially, we analyzed participant characteristics using descriptive statistics. This study utilized SPSS version 26 to conduct independent sample t-Test and One-way ANOVA to determine whether religious beliefs (RB), fear of COVID-19 (FoC), and well-being (WB) had statistically significant differences.
Smart partial least squares (Smart PLS)-SEM analysis, a variance-based structural equation modeling [58] in the most recent version of Smart PLS 4.0 was utilized to analyze the data gathered for this study. PLS-SEM approach was selected to validate the hypotheses of the study and was used to analyze the effects of the independent variables on the dependent variables and examine the mediation hypothesis.
The technique for using the PLS-SEM methodology systematically included analyzing the measurement model and structural model. Reflective indicator reliability (outer loading), construct reliability, convergent validity, and discriminant validity were tested for the goal of evaluating the measurement model. The collinearity statistics variance inflation factor (VIF), the coefficient determination (R2), and the effect size f2 were evaluated in the structural model. We conducted a multiple-mediated PLS path model with WB as the input variable, RB as the mediating variable and FoC as the output variable.
Results of independent sample t-Test and One-way ANOVA
An Independent Sample t-Test was conducted to compare FoC and WB in terms of gender and in terms of history of chronic disease, as shown in Table 2.
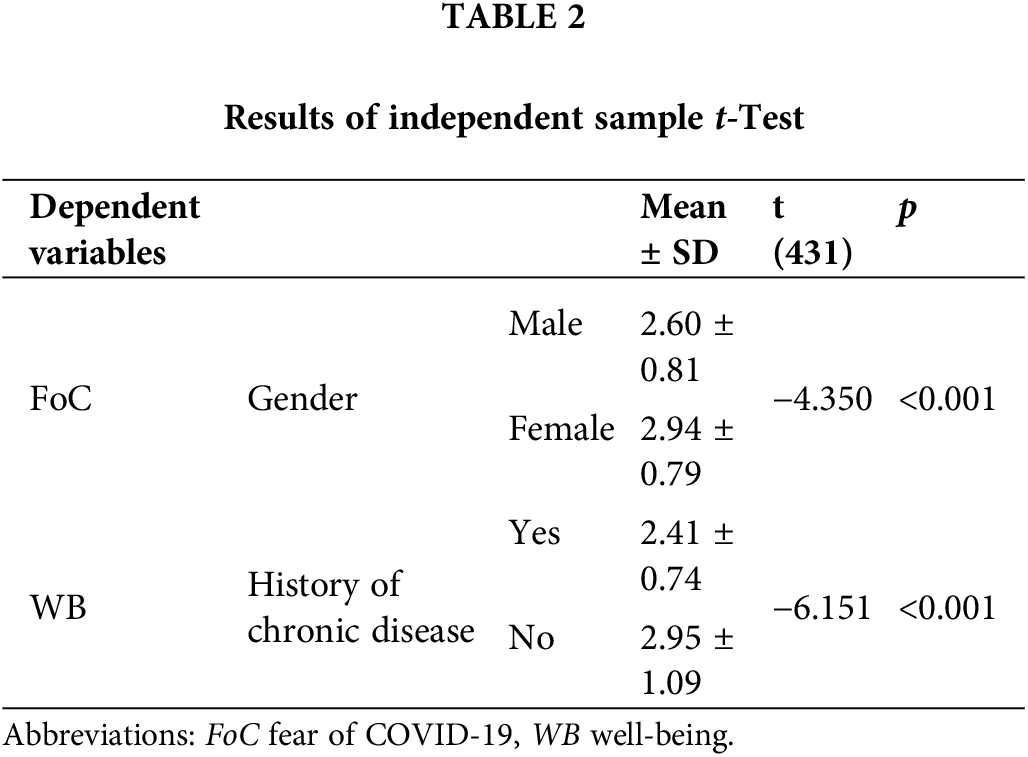
The amount of fear of COVID-19 differed significantly between males and females, t (431) = −4.350, p = 0.000. As a result, females (M = 2.94, SD = 0.79) experienced more fear of COVID-19 than males (M = 2.60, SD = 0.81) (H1 accepted). The level of well-being had differed significantly between people without history of chronic disease (M = 2.95; SD = 1.09) and people with a history of chronic disease (M = 2.41; SD = 0.74); t (431) = −6.151, p = 0.000. These results suggested that individuals without chronic disease had higher levels of well-being than individuals with chronic disease (H2 accepted).
The differences between frequency of religious attendance, age and WB; between frequency of religious attendance, age and RB were performed by One-way ANOVA, as presented in Table 3. If Levene’s test is significant, the homogeneity of variance assumption needed for an ANOVA is met. In contrast, Welch’s adjusted F ratio is employed to correct for violating the assumption of homogeneity of variance.
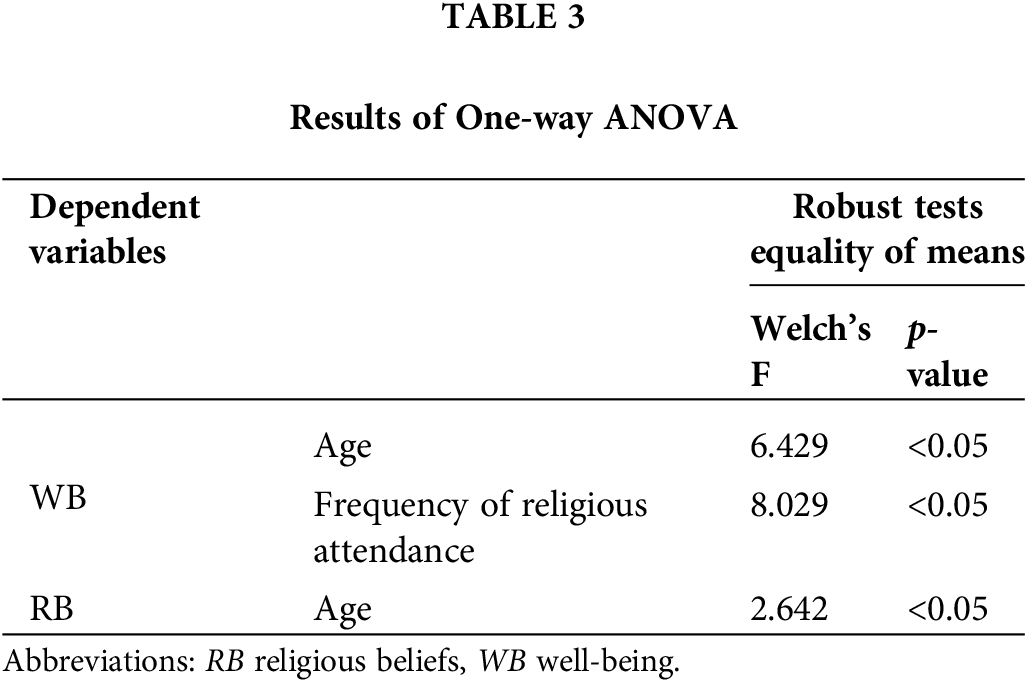
The outcome of Levene’s Test showed is not significant of frequency of religious attendance [F(5,427) = 4.269, p < 0.05] and age [F(5,427) = 9.54, p < 0.05] according to WB. Therefore, Welch’s adjusted F ratio was employed, revealing significant differences of age [Welch’s F(5,122) = 6.429, p < 0.05] and frequency of religious attendance [Welch’s F(5,156) = 8.029, p < 0.05]. The findings showed that individuals who attended religious services daily (M = 3.47, SD = 0.81) had higher levels of WB than individuals who attended religious services several times a week (M = 3.03, SD = 0.92); once a week (M = 2.48, SD = 0.93); several times in one month (M = 2.53, SD = 0.85); once a month or less (M = 2.67, SD = 0.93) and never attend (M = 2.77, SD = 1.22) (H3 accepted). While, individuals from the age of 18–20 (M = 3.04, SD = 1.15) and 21–30 (M = 3.01, SD = 1.12) had higher levels of WB than individuals from 31 to above 60 years (H4 rejected).
The outcome of Levene’s Test showed is no significance of age [F(5,427) = 2.63, p < 0.05] in terms of RB. Therefore, Welch’s adjusted F ratio was employed, revealing a significant age difference [Welch’s F(5,121) = 2.642, p < 0.05]. The finding showed that individuals aged 51 to 60 (M = 3.2, SD = 0.86) and above 60 (M = 3.29, SD = 0.77) had higher RB than individuals from 18 to 50 years (H5 accepted).
Indicator Reliability (Outer loading): In the present study, most of the outer loadings above 0.708 met the criteria for indicator reliability. The remaining indicators with loadings ranging from 0.4 to 0.7 were accepted [59]. The elimination of these indicators did not lead to the improvement of CR and AVE, as referred in Table 4.
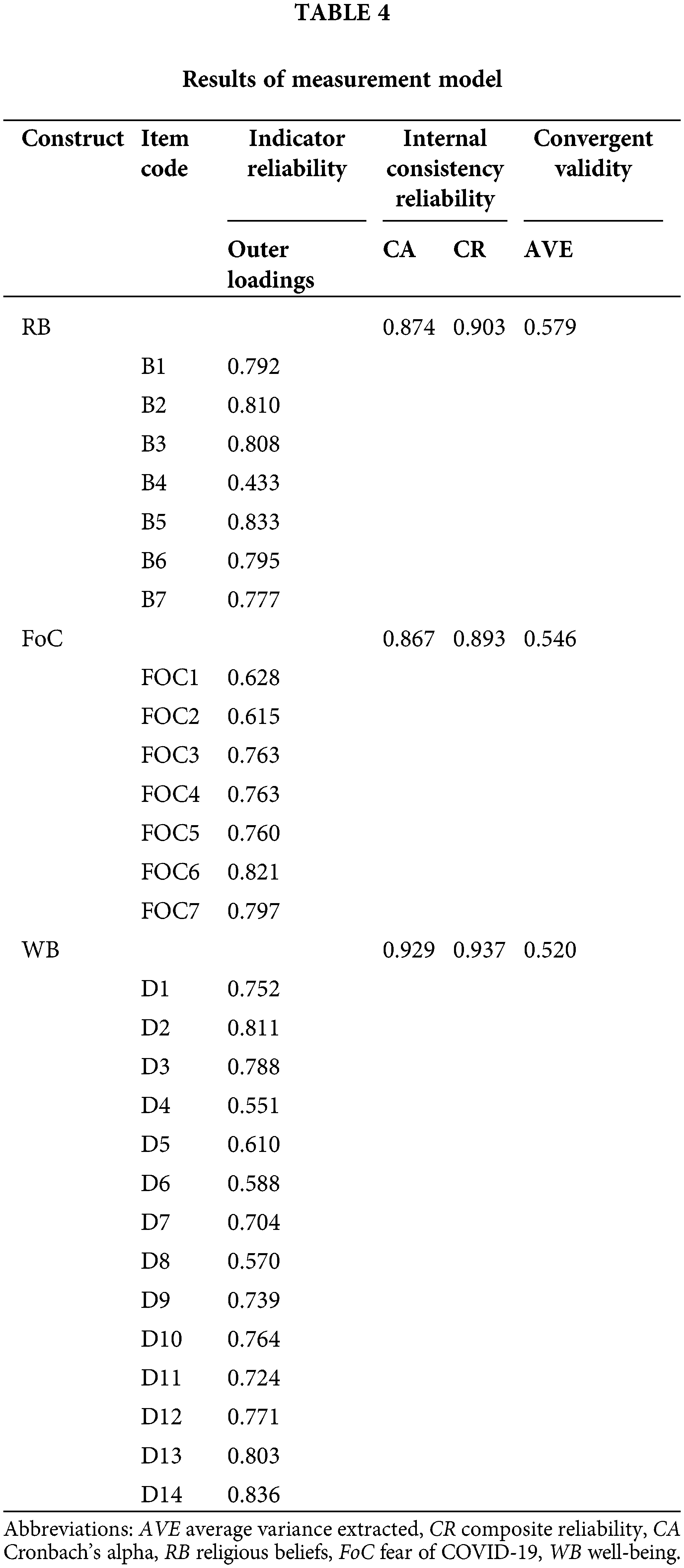
Construct Reliability (CA; CR): The results for CA and CR are presented in Table 4 for RB (0.874, 0.903), FoC (0.867, 0.893), WB (0.929, 0.937), respectively. This study found the reliability values to be in a satisfactory range [59].
Convergent Validity (AVE): AVE values for RB, FoC and WB were 0.579, 0.546, 0.520, respectively (shown in Table 4). All the values were greater than the 0.50 threshold, which was acceptable [59].
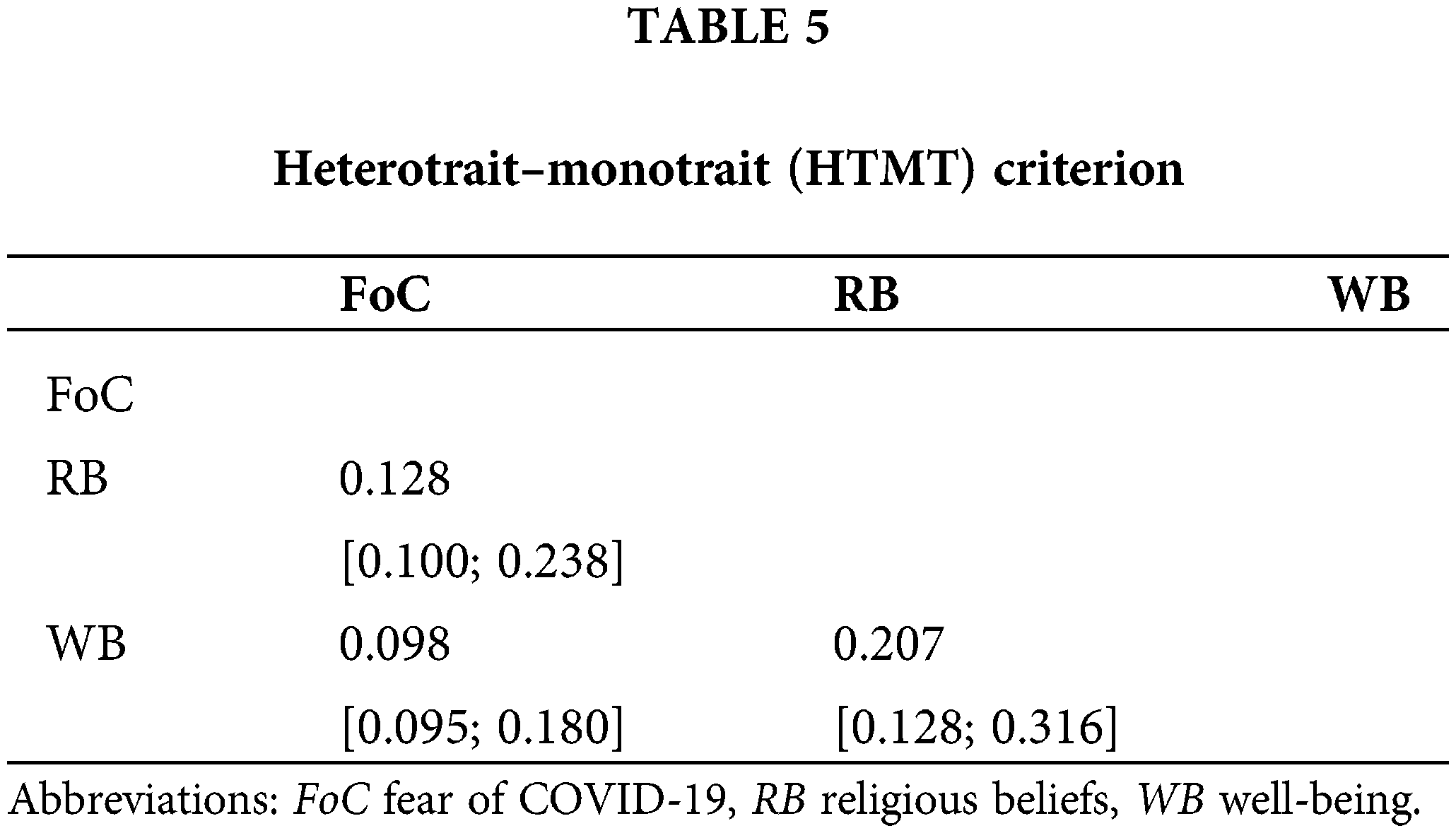
Discriminant Validity (HTMT): Bootstrap confidence intervals can test if the HTMT is significantly different from 1.0 [60] and the HTMT ratio results were lower than the 0.85 thresholds, which were presented in Table 5.
Assessment of structural model
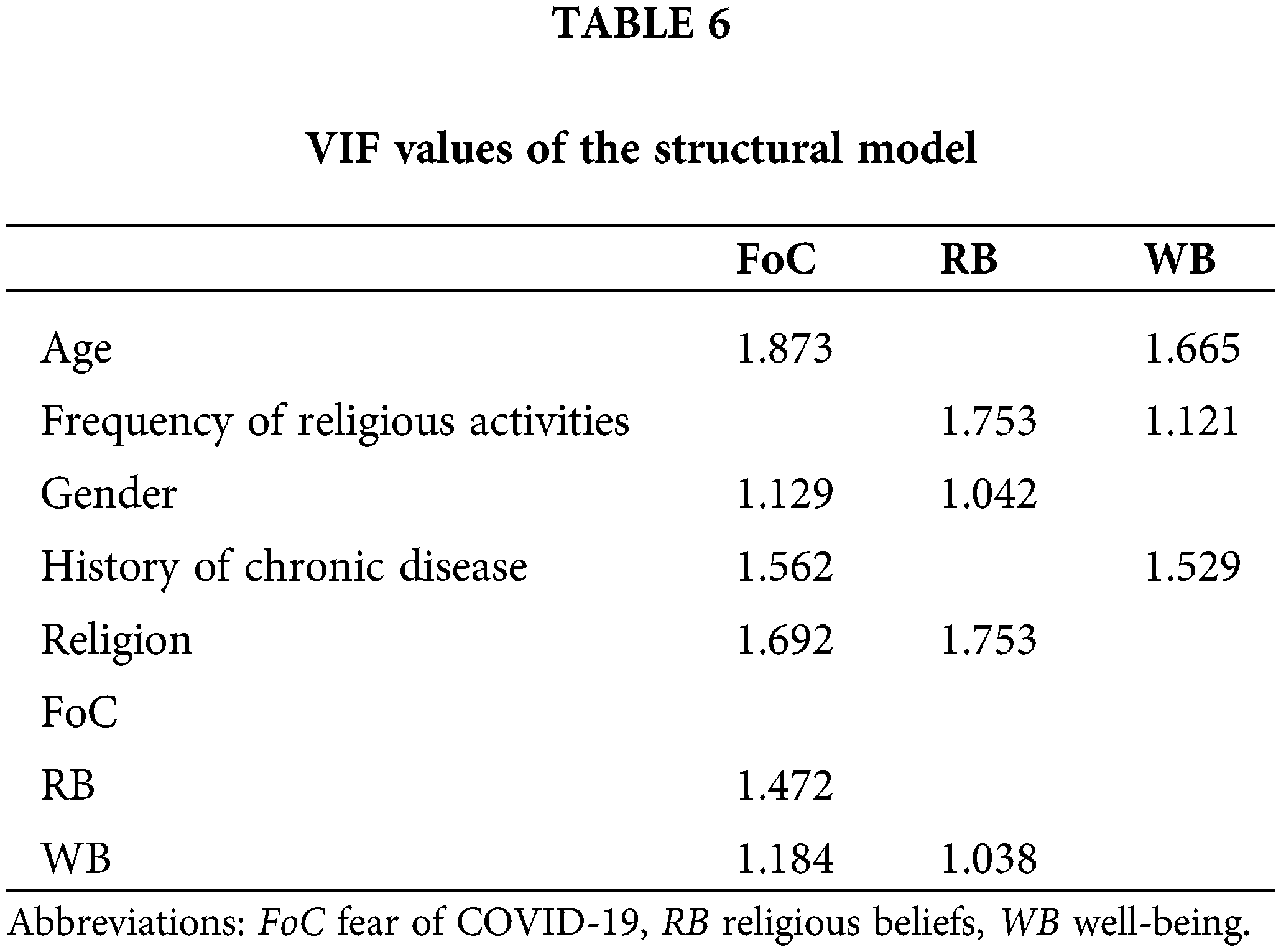
Collinearity statistics (VIF): The values of VIF are equal to or less than 3.30 considered biased free [61]. All VIF values were less than 3.30 concluding that the data set was not suffered from a common bias issue in achieved data (referred to Table 6).
Coefficient of determination (R2): The R2 ranges from 0 to 1, with higher values indicating a greater explanatory power [59]. The values of R2 must be higher than 0.1 is considerable [62]. In our study, the R2 value 0.127 depicts that WB and RB together caused 12.7% variance in FoC (referred to Table 7).
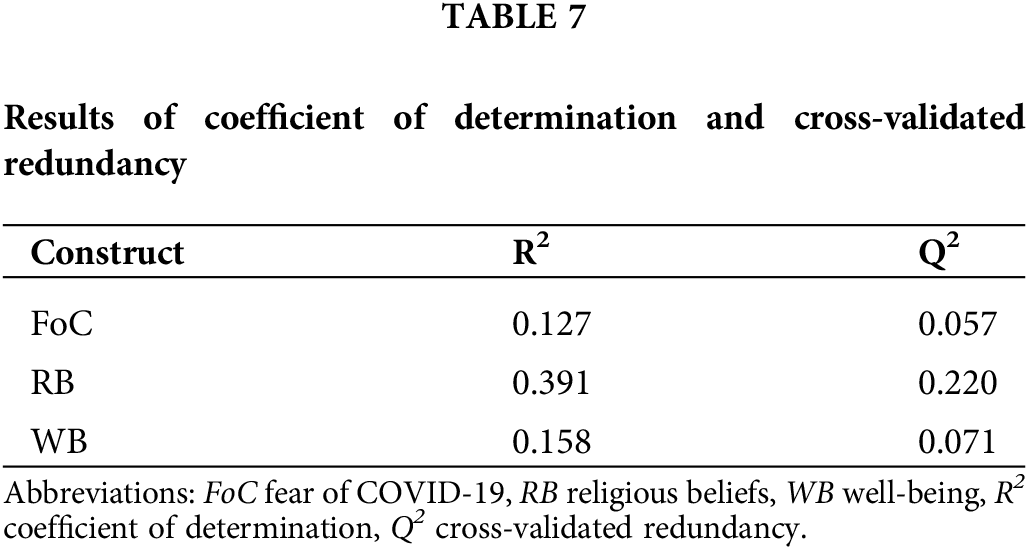
Cross-validated redundancy (Q2): The Q2 values of FoC, RB, WB were 0.057, 0.220 and 0.071 respectively, indicating the predictive relevance of the present study model [63,64] (refer to Table 7).
The effect sizes (f2): The effect size of f2 showed relatively small effects of RB on FoC (0.031) and WB on RB (0.023) and there was no effect of WB on FoC (less than 0.02) [61,64].
The final model of PLS is presented in Fig. 1. In the mediation model, WB and RB mediated the effects of history of chronic disease, frequency of religious attendance, gender, and religion on the FoC. We found that 12.7% of the variance in the FoC was explained by RB, history of chronic disease, gender, age and religion, while WB had no significant impact. PLS showed that 15.8% of the variance in the WB could be explained by the regression on history of chronic disease, frequency of religious activities and age, while 39.1% of the variance in the RB was explained by WB, gender, frequency of religious activities and religion. The effect of WB on the FoC was mediated by RB.
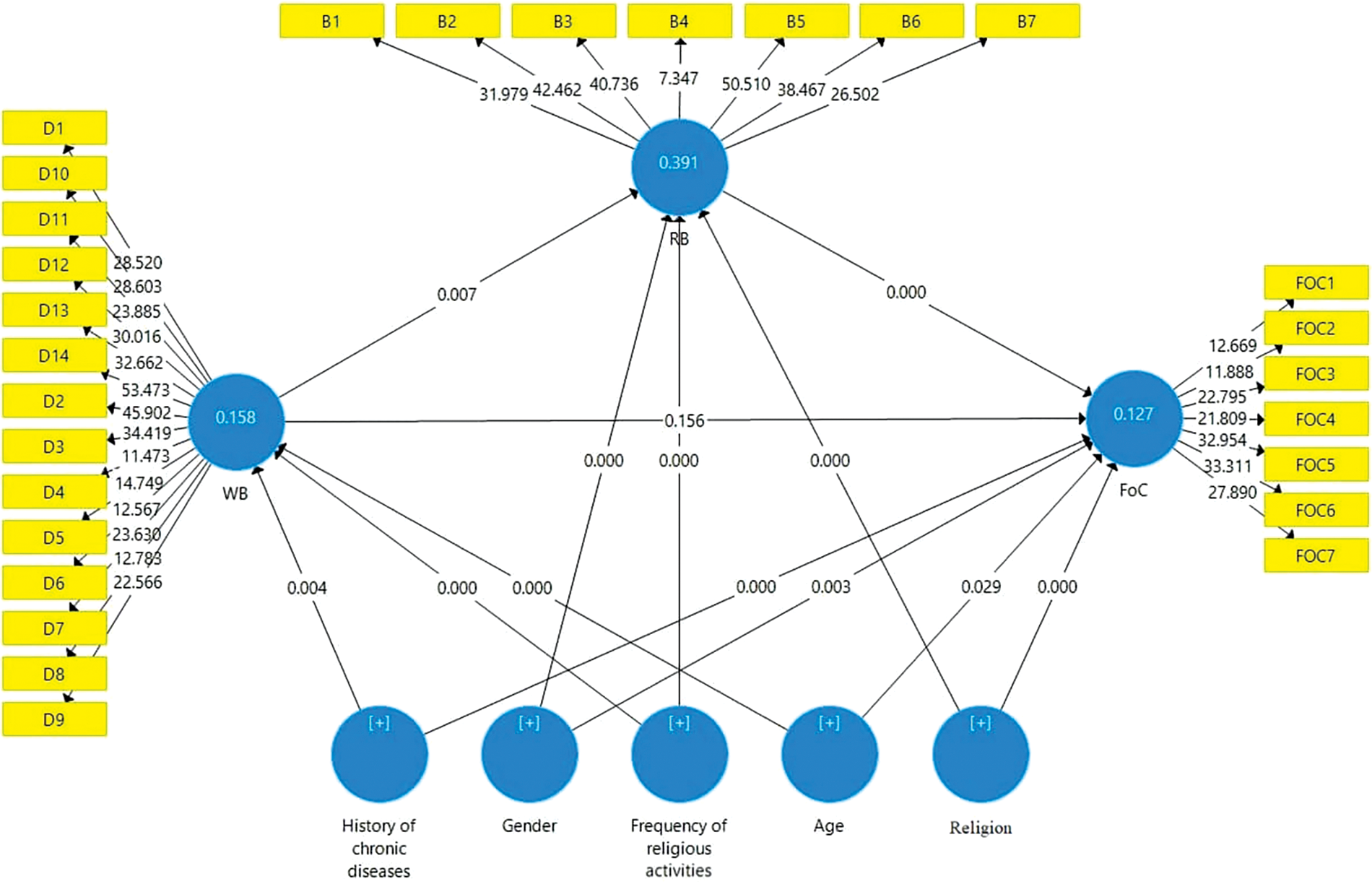
Figure 1: A structural model.
The results from Table 8 showed that negative effects of age on FoC (β = −0.153; t = 2.180; p = 0.029) and WB (β = −0.283; t = 4.865; p < 0.001), frequency of religious activities had positive effects on RB (β = 0.350; t = 6.420; p < 0.001) and WB (β = 0.239; t = 4.937; p < 0.001), gender had positive effects on FoC (β = 0.153; t = 3.029; p = 0.003) and RB (β = 0.232; t = 5.754; p < 0.001). There was a negative effect of history of chronic disease (β = −0.227; t = 3.623; p < 0.001) on FoC and a positive effect on WB (β = 0.157; t = 2.926; p = 0.004). Besides, the findings indicated that religion had a positive effect on FoC (β = 0.225; t = 4.122; p < 0.001) and a negative effect of religion on RB (β = −0.303; t = 6.105; p < 0.001).
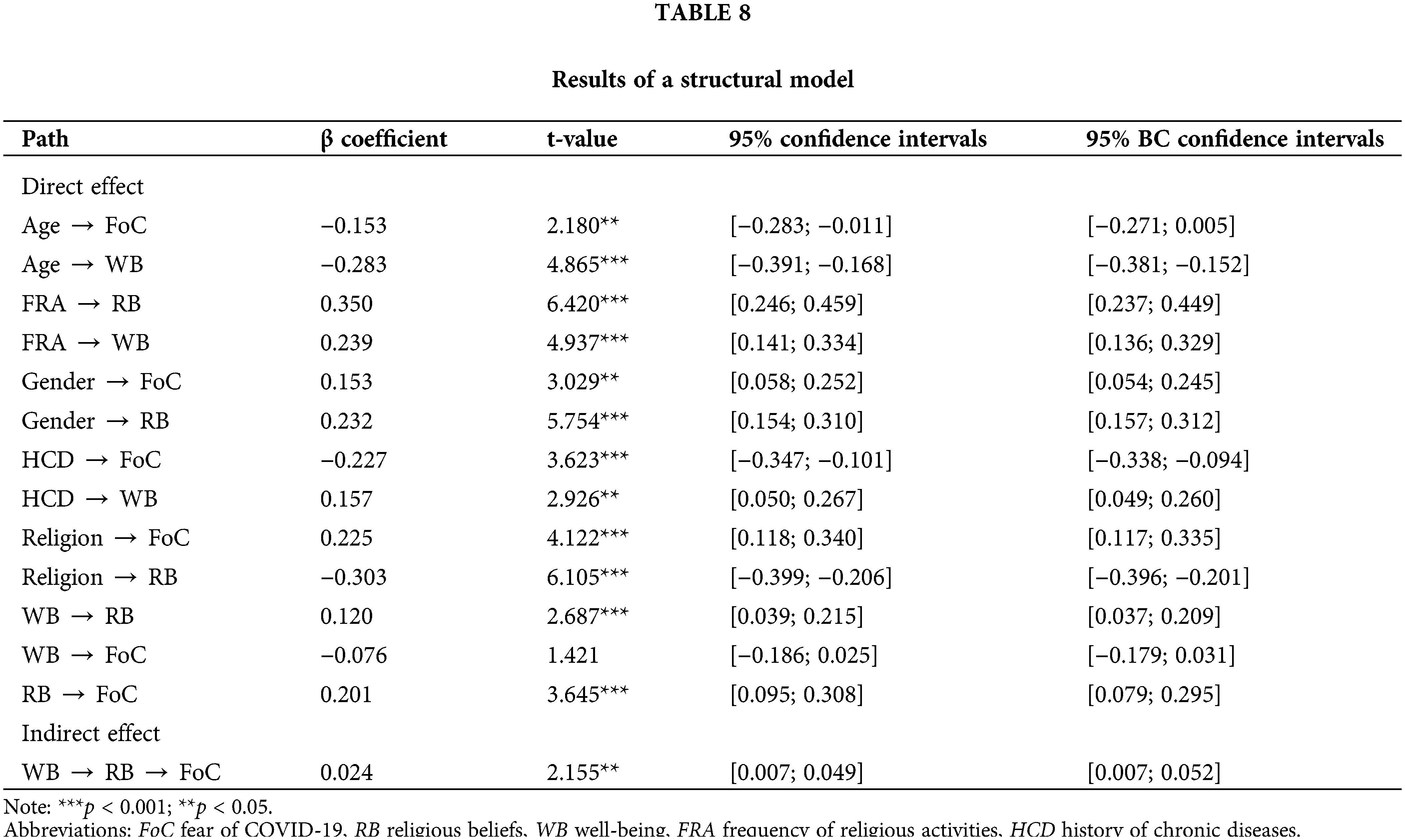
The results showed that the direct effect of WB on FoC was not significant (β = −0.076, t = 1.421, p = 0.156). The findings revealed a positive effect of WB on RB (β = 0.120; t = 2.687; p < 0.001), and a positive effect of RB on FoC (β = 0.201; t = 3.645; p < 0.001) (H6 rejected). The results also showed that the indirect effect of RB between the relationship WB and FoC was positive and statistically significant (β = 0.024, t = 2.155, p = 0.031). The present study signaled a full mediation effect [65]. This result suggested that RB mediated the effect of WB on FoC (H7 accepted).
The current study provides existing research on mental health support that may protect against the influence on the COVID-19 crisis by investigating relations between well-being, religious beliefs and fear of COVID-19. Our study highlighted a few significant findings.
According to our findings, females experience more fear of COVID-19 than males. Our result ties well with previous studies wherein the pandemic causes more psychological effects in females [26,66,67]. Females were physically weaker and sicker more often [68], they experienced more fear of COVID-19 compared to males since they got sick. Besides, females had more caregiver responsibilities than usual [69]; were more likely to regard the pandemic as a major health concern and more risk-averse than males [70].
This study shows people without chronic disease experience more well-being than people with chronic disease. The findings in these prior analyses are similar to what we observed in our models, individuals without chronic disease have much greater well-being than people with chronic disease [27,29]. People with chronic diseases have been considered susceptible populations under tremendous physical and psychological stress, fear and anxiety about being infected in a public health crisis [71,72]. They were more at risk of contagion and the consequences were more severe.
The present research findings indicate that individuals who attend religious services daily experience more well-being than those who hardly or never attend. This result is consistent with research that reported a positive relationship between religious services attendance and well-being [37,38]. Many prior scholars reported that attending religious services enhanced social integration, belonging, peacefulness, hope and released negative emotions [39,73].
Our data analysis reveals a difference between age and well-being, reflecting younger adults experience more well-being levels than middle and older adults. This is a surprising finding, contrary to what we know from prior findings [43,44], which have shown that older adults experience more well-being than younger adults. Like many Asian countries, the majority of Vietnamese elderly often live with later generations in large families [74,75]. Particularly in the COVID-19 pandemic, household income declined, resulting in reduced support from offspring and relatives to older people. Specifically, households with older people needing medical care could temporarily fall into poverty because of COVID-19 [76]. Although the national social security organization paid benefits and provided home care programs for the elderly, older people worried that they would be unable to support their offspring and would become a hindrance to their loved ones.
The present result is in line with a study showing that older adults have higher levels of religiosity than younger adults [48]. During old age, the major negative influences are acute and chronic physical health issues, the loss of roles in society and family, financial stresses, loss of loved ones, and problems related to suffering and death. Older adults frequently have depleted personal resources to deal and tend to handle difficulties including looking for social support and positive reappraisal. Many older people reported that religious beliefs help them cope with physical health problems and life stresses, manage loneliness, purpose and meaning of life, especially in COVID-19 [77].
We found that religious beliefs positively predict the fear of COVID-19, which individuals with high levels of religious beliefs are associated with increased fear of COVID-19. Previous research showed that frequency of religious attendance improved the mental health of religious believers [78]. Religious beliefs and practices were related to the ability to cope with the disease and a positive attitude in a difficult situation [79]. However, it should be noted that the meanings of death, suffering, and so on are highly subjective and determined by personal interpretations of religious teachings and hence these meanings are not always positive in terms of mental health.
In the context of COVID-19, social distancing and other restrictions leading to a lack of religious communication can prevent proper assistance and guidance from religious leaders as well as the community, which may increase the likelihood of related misperceptions and negative emotions [80]. Religious believers experience feelings of anger toward, of abandonment and have difficulty reconciling their belief in a loving God, Buddha with the suffering generated by the pandemic and questions about the ultimate meaning and purpose of life, among other issues.
We discovered that religious beliefs in fact fully mediate the effects of well-being on the fear of COVID-19, indicating that religious beliefs act indirectly in the fear of COVID-19. The dimension of religious beliefs positively and significantly mediate the relationship between well-being and the fear of COVID-19. People who experience higher levels of well-being are more likely to have higher levels of religious beliefs, which leads to more fear of COVID-19. Previous models have not examined role of religious beliefs in mediating the relationship between well-being and the fear of COVID-19, more targeted interventions should be developed in further research.
The current study has some limitations. First, the study is conducted through an online survey, which is associated with low participation of the elderly and technologically disadvantaged people, reducing the generalizability of the results to a representative population. Larger and more representative groups of the population are needed to increase the accuracy of the findings and explore more factors related to school-education, socio-economic status and employment status, which may be considered in future studies. Second, the recent study do not address religious well-being or religious coping, limiting the scope of the findings. Further studies should investigate the role of religious coping and religious well-being in fear of COVID-19.
Effective positive psychological interventions and support strategies should be implemented to enhance psychological resilience and improve the population’s mental health, especially religious aspects. Religious beliefs have not only helped in spiritual attainment of salvation but also in physical health and temporal longevity among the elderly. Religious strategies have been proven to support older adults in coping with loneliness, purpose, meaning of life, physical limitations and losses.
For clinical practices, our results recommend that clinicians should consider the role of religion into the treatment to support well-being and mental health of clients during a public health crisis. Flaxman et al. [81] found that people who had higher levels of religiosity reported higher psychological therapy benefits, specifically concerning coping skills. Clinicians are encouraged to learn about religiously integrated psychotherapy approaches so that they can support clients within their current transcendental belief systems.
According to Cognitive Behavior Therapy (CBT), religion has a role in developing “cognitive schemata” and a religious framework that can operate as a generic mental model, contributing to a consistent and adaptive assessment of situations [82]. Besides, Acceptance and Commitment Therapy (ACT) plays an important part in stimulating the third wave of behavior therapy and be recently practiced in clinical settings [83]. According to ACT, clients are guided to accept what cannot be changed and adapt their behavior regarding the issues. The goal of ACT is to assist individuals in living with psychological suffering, clarifying and committing to personal values, like region. ACT appears to be an appropriate method for the variety of COVID-related stress: through focusing on the main adaptive processes that underpin psychological health and resilience [84,85].
Online interventions developed and implemented by mental health professionals might improve people’s ability to cope with stressors throughout adversity [86]. Most clients tend to find out an app that can give individualized healthcare advice or treatments as access to physical and mental healthcare during COVID-19. Mobile Health (mHealth) applications have appeared to be a useful approach for disease and health management, enhancing healthcare services’ effectiveness [84]. Specifically, mHealth applications can potentially help prevent the spread of contagious diseases in society by using distance communication [85] to massively implement these applications in all healthcare settings [86]. Mental health hotlines should be developed throughout Vietnam and provided the public with counseling and psychological services to share strategies, recommendations, and education programs for dealing with potential mental disorders. In response to these issues, and recognizing that many people do not know where to turn for mental health support, a directory of services for Vietnamese communities has been compiled by mental health experts in Vietnam.
The data points to a decrease in well-being in middle and older adults and people with chronic diseases. The findings of the present study indicate that females have a relatively higher level of fear of COVID-19 than males. These findings may be helpful for healthcare providers who should consider strategies, build awareness of mental health needs for improving preventive behaviors among older adults, people with chronic disease and females to help them ease their worries and fears concerning COVID-19. Family support, social support, early detection of mental distress, and interventions should be implemented to alleviate mental health issues and reduce feelings of isolation and social maladaptation. The present study finds that religious attendance has the potential protection regarding Vietnamese mental health. Clinicians and therapists should consider integrating religion into clinical interventions and treatment to improve clients’ mental health. Individuals who engage in religious services daily would experience more well-being than those who hardly and never attend. Our study demonstrates that religious beliefs mediate the association between well-being and fear of COVID-19. These religious beliefs increase fear of disease. Healthcare professionals should be aware of both the positive and negative uses of individuals’ beliefs to provide the most comprehensive care possible.
Acknowledgement: We appreciate the support of participants in data collecting.
Funding Statement: The authors received no specific funding for this study.
Author Contributions: The authors confirm contribution to the paper as follows: study conception and design: Van-Son Huynh, Gallayaporn Nantachai, Vinh-Long Tran-Chi; data collection: Xuan Thanh Kieu Nguyen, Vinh-Long Tran-Chi; analysis and interpretation of results: Vinh-Long Tran-Chi, Thanh-Thao Ly, My-Tien Nguyen-Thi, Xuan Thanh Kieu Nguyen; draft manuscript preparation: Vinh-Long Tran-Chi, Thanh-Thao Ly, My-Tien Nguyen-Thi, Xuan Thanh Kieu Nguyen. All authors reviewed the results and approved the final version of the manuscript.
Ethics Approval: The present study adhered to the Declaration of Helsinki regarding research on human participants. The study was approved by the Ethic Committee of the Department of Science and Technology—Ho Chi Minh City University of Education (under the Vietnamese MoET) with 420 number NV2021.19.02.DH on June 01, 2021.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
References
1. Quach HL, Hoang NA. COVID-19 in Vietnam: a lesson of pre-preparation. J Clin Virol [Internet]. 2020;127:104379. doi:https://doi.org/10.1016/j.jcv.2020.104379. [Google Scholar] [PubMed] [CrossRef]
2. Hoang VT, Pham TD, Nguyen QT, Nguyen DC, Nguyen DT, Nguyen TB, et al. Seroprevalence of SARS-CoV-2 among high-density communities and hyper-endemicity of COVID-19 in Vietnam. Trop Med Int Health [Internet]. 2022;27(5):515–21. doi:https://doi.org/10.1111/tmi.13744. [Google Scholar] [PubMed] [CrossRef]
3. Information about coronavirus diease outbreak COVID-19 [in Vietnamese] [Internet]. 2021. https://ncov.moh.gov.vn/ [cited 4th January 2022]. [Google Scholar]
4. Cooke JE, Eirich R, Racine N, Madigan S. Prevalence of posttraumatic and general psychological stress during COVID-19: a rapid review and meta-analysis. Psychiat Res [Internet]. 2020;292:113347. doi:https://doi.org/10.1016/j.psychres.2020.113347. [Google Scholar] [PubMed] [CrossRef]
5. Xafis V. What is inconvenient for you is life-saving for me’: how health inequities are playing out during the COVID-19 pandemic. Asian Bioeth Rev [Internet]. 2020;12(2):223–34. doi:https://doi.org/10.1007/s41649-020-00119-1. [Google Scholar] [PubMed] [CrossRef]
6. Banerjee D. The COVID-19 outbreak: crucial role the psychiatrists can play. Asian J Psychiatr [Internet]. 2020;50. [Google Scholar]
7. Luchetti M, Lee JH, Aschwanden D, Sesker A, Strickhouser JE, Terracciano A, et al. The trajectory of loneliness in response to COVID-19. Am Psychol [Internet]. 2020;75(7):897–908. doi:https://doi.org/10.1037/amp0000690. [Google Scholar] [PubMed] [CrossRef]
8. Cherry KE, Sampson L, Nezat PF, Cacamo A, Marks LD, Galea S. Long-term psychological outcomes in older adults after disaster: relationships to religiosity and social support. Aging Ment Health [Internet]. 2015;19(5):430–43. doi:https://doi.org/10.1080/13607863.2014.941325. [Google Scholar] [PubMed] [CrossRef]
9. Aten JD, Smith WR, Davis EB, van Tongeren DR, Hook JN, Davis DE, et al. The psychological study of religion and spirituality in a disaster context: a systematic review. Psychol Trauma: Theory Res Pract Policy [Internet]. 2019;11(6):597–613. doi:https://doi.org/10.1037/tra0000431. [Google Scholar] [PubMed] [CrossRef]
10. Walsh F. Loss and resilience in the time of COVID-19: meaning making, hope, and transcendence. Fam Process [Internet]. 2020;59(3):898–911. doi:https://doi.org/10.1111/famp.12588. [Google Scholar] [PubMed] [CrossRef]
11. Ellison CG, Boardman JD, Williams DR, Jackson JS. Religious involvement, stress, and mental health: findings from the 1995 Detroit area study. Soc Forces [Internet]. 2001;80(1):215–49. doi:https://doi.org/10.1353/sof.2001.0063. [Google Scholar] [CrossRef]
12. Prime H, Wade M, Browne DT. Risk and resilience in family well-being during the COVID-19 pandemic. Am Psychol [Internet]. 2020;75(5):631–43. doi:https://doi.org/10.1037/amp0000660. [Google Scholar] [PubMed] [CrossRef]
13. Chidarikire S, Cross M, Skinner I, Cleary M. An ethnographic study of schizophrenia in Zimbabwe: the role of culture, faith, and religion. J Spiritual Ment [Internet]. 2020;22(2):173–94. doi:https://doi.org/10.1080/19349637.2018.1531366. [Google Scholar] [CrossRef]
14. Wang J, Wang JX, Yang GS. The psychological impact of COVID-19 on Chinese individuals. Yonsei Med J [Internet]. 2020;61(5):438–40. doi:https://doi.org/10.3349/ymj.2020.61.5.438. [Google Scholar] [PubMed] [CrossRef]
15. Adolphs R. The biology of fear. Curr Biol [Internet]. 2013;23(2):R79–93. doi:https://doi.org/10.1016/j.cub.2012.11.055. [Google Scholar] [PubMed] [CrossRef]
16. Bakioğlu F, Korkmaz O, Ercan H. Fear of COVID-19 and positivity: mediating role of intolerance of uncertainty, depression, anxiety, and stress. Int J Ment Health Addict [Internet]. 2021;19(6):2369–82. doi:https://doi.org/10.1007/s11469-020-00331-y. [Google Scholar] [PubMed] [CrossRef]
17. Pakpour AH, Griffiths MD, Lin CY. Assessing psychological response to the COVID-19: the fear of COVID-19 scale and the COVID stress scales. Int J Ment Health Addict [Internet]. 2021;19(6):2407–10. doi:https://doi.org/10.1007/s11469-020-00334-9. [Google Scholar] [PubMed] [CrossRef]
18. Henrich J, Bauer M, Cassar A, Chytilová J, Purzycki B. War increases religiosity. Nat Hum Behav [Internet]. 2019;3(2):129–35. doi:https://doi.org/10.1038/s41562-018-0512-3. [Google Scholar] [PubMed] [CrossRef]
19. Francis B, Ken CS, Han NY, Ariffin MAA, Yusuf MHM, Wen LJ, et al. Religious coping during the COVID-19 pandemic: gender, occupational and socio-economic perspectives among Malaysian frontline healthcare workers. Alpha Psychol [Internet]. 2021;22(4):194–9. doi:https://doi.org/10.5152/alphapsychiatry.2021.21185. [Google Scholar] [PubMed] [CrossRef]
20. Bentzen JS. In crisis, we pray: religiosity and the COVID-19 pandemic. J Econ Behav Organ [Internet]. 2021;192(1):541–83. doi:https://doi.org/10.1016/j.jebo.2021.10.014. [Google Scholar] [PubMed] [CrossRef]
21. Enea V, Eisenbeck N, Petrescu TC, Carreno DF. Perceived impact of quarantine on loneliness, death obsession, and preoccupation with God: predictors of increased fear of COVID-19. Front Psychol [Internet]. 2021;12:643977. doi:https://doi.org/10.3389/fpsyg.2021.643977. [Google Scholar] [PubMed] [CrossRef]
22. Chen Y, Kim ES, VanderWeele TJ. Religious-service attendance and subsequent health and well-being throughout adulthood: evidence from three prospective cohorts. Int J Epidemiol [Internet]. 2020;49(6):2030–40. doi:https://doi.org/10.1093/ije/dyaa120. [Google Scholar] [PubMed] [CrossRef]
23. Tolin DF, Foa EB. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Trauma: Theory Res Pract Policy [Internet]. 2008;S(1):37–85. doi:https://doi.org/10.1037/1942-9681.S.1.37. [Google Scholar] [CrossRef]
24. Vlassoff C. Gender differences in determinants and consequences of health and illness. J Health Popul Nutr [Internet]. 2007;25(1):47–61. [Google Scholar] [PubMed]
25. Alsharawy A, Spoon R, Smith A, Ball S. Gender differences in fear and risk perception during the COVID-19 pandemic. Front Psychol [Internet]. 2021;12:3104. [Google Scholar]
26. van Nghia H. Religious diversity and the right to freedom of religion in Vietnam today. Acad J Interdiscip Stud [Internet]. 2015;4(1):213–22. doi:https://doi.org/10.5901/mjss.2015.v4n1p213. [Google Scholar] [CrossRef]
27. Ozamiz-Etxebarria N, Dosil-Santamaria M, Picaza-Gorrochategui M, Idoiaga-Mondragon N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad Saude Publica [Internet]. 2020;36(4):1–9. [Google Scholar]
28. Rapelli G, Lopez G, Donato S, Pagani AF, Parise M, Bertoni A, et al. A postcard from Italy: challenges and psychosocial resources of partners living with and without a chronic disease during COVID-19 epidemic. Front Psychol [Internet]. 2020;11:567522. doi:https://doi.org/10.3389/fpsyg.2020.567522. [Google Scholar] [PubMed] [CrossRef]
29. Burr DA, Castrellon JJ, Zald DH, Samanez-Larkin GR. Emotion dynamics across adulthood in everyday life: older adults are more emotionally stable and better at regulating desires. Emotion [Internet]. 2021;21(3):453–64. doi:https://doi.org/10.1037/emo0000734. [Google Scholar] [PubMed] [CrossRef]
30. Koenig LB, Vaillant GE. A prospective study of church attendance and health over the lifespan. Health Psychol [Internet]. 2009;28(1):117–24. doi:https://doi.org/10.1037/a0012984. [Google Scholar] [PubMed] [CrossRef]
31. Sternthal MJ, Williams DR, Musick MA, Buck AC. Depression, anxiety, and religious life: a search for mediators. J Health Soc Behav [Internet]. 2010;51(3):343–59. doi:https://doi.org/10.1177/0022146510378237. [Google Scholar] [PubMed] [CrossRef]
32. Koenig HG. Religious attitudes and practices of hospitalized medically ill older adults. Int J Geriatr Psychiatry [Internet]. 1998;13(4):213–24. doi:https://doi.org/10.1002/(ISSN)1099-1166. [Google Scholar] [CrossRef]
33. Jones JW. Religion, health, and the psychology of religion: how the research on religion and health helps us understand religion. J Relig Health [Internet]. 2004;43(4):317–28. doi:https://doi.org/10.1007/s10943-004-4299-3. [Google Scholar] [CrossRef]
34. Graham C, Crown S. Religion and well-being around the world: social purpose, social time, or social insurance? Int J Wellbeing [Internet]. 2014;4(1):1–27. doi:https://doi.org/10.5502/ijw.v4i1.1. [Google Scholar] [CrossRef]
35. Klokgieters SS, van Tilburg TG, Deeg DJ, Huisman M. Do religious activities among young-old immigrants act as a buffer against the effect of a lack of resources on well-being? Aging Ment Health [Internet]. 2019;23(5):625–32. doi:https://doi.org/10.1080/13607863.2018.1430739. [Google Scholar] [PubMed] [CrossRef]
36. Osei-Tutu A, Affram AA, Mensah-Sarbah C, Dzokoto VA, Adams G. The impact of COVID-19 and religious restrictions on the well-being of Ghanaian Christians: the perspectives of religious leaders. J Relig Health [Internet]. 2021;60(4):2232–49. doi:https://doi.org/10.1007/s10943-021-01285-8. [Google Scholar] [PubMed] [CrossRef]
37. Greenfield EA, Marks NF. Religious social identity as an explanatory factor for associations between more frequent formal religious participation and psychological well-being. Int J Psychol Relig [Internet]. 2007;17(3):245–59. doi:https://doi.org/10.1080/10508610701402309. [Google Scholar] [PubMed] [CrossRef]
38. Hill TD. Religion, spirituality, and healthy cognitive aging. Spirituality/Medicine Interface Project [Internet]. 2006;99(10):1176–7. doi:https://doi.org/10.1097/01.smj.0000242747.71884.66. [Google Scholar] [PubMed] [CrossRef]
39. Michaels JL, Hao F, Ritenour N, Aguilar N. Belongingness is a mediating factor between religious service attendance and reduced psychological distress during the COVID-19 pandemic. J Relig Health [Internet]. 2022;61(2):1750–64. doi:https://doi.org/10.1007/s10943-021-01482-5. [Google Scholar] [PubMed] [CrossRef]
40. Stone AA, Schwartz JE, Broderick JE, Deaton A. A snapshot of the age distribution of psychological well-being in the United States. Proc Natl Acad Sci [Internet]. 2010;107(22):9985–90. doi:https://doi.org/10.1073/pnas.1003744107. [Google Scholar] [PubMed] [CrossRef]
41. Aizpurua A, Migueles M, Aranberri A. Prospective memory and positivity bias in the COVID-19 health crisis: the effects of aging. Front Psychol [Internet]. 2021;12:2532. doi:https://doi.org/10.3389/fpsyg.2021.666977. [Google Scholar] [PubMed] [CrossRef]
42. Carstensen LL, Shavit YZ, Barnes JT. Age advantages in emotional experience persist even under threat from the COVID-19 pandemic. Psychol Sci [Internet]. 2020;31(11):1374–85. doi:https://doi.org/10.1177/0956797620967261. [Google Scholar] [PubMed] [CrossRef]
43. Bidzan-Bluma I, Bidzan M, Jurek P, Bidzan L, Knietzsch J, Stueck M, et al. A polish and German population study of quality of life, well-being, and life satisfaction in older adults during the COVID-19 pandemic. Front Psychiatry [Internet]. 2020;11:1188. doi:https://doi.org/10.3389/fpsyt.2020.585813. [Google Scholar] [PubMed] [CrossRef]
44. Birditt KS, Turkelson A, Fingerman KL, Polenick CA, Oya A. Age differences in stress, life changes, and social ties during the COVID-19 pandemic: implications for psychological well-being. Gerontologist [Internet]. 2021;61(2):205–16. doi:https://doi.org/10.1093/geront/gnaa204. [Google Scholar] [PubMed] [CrossRef]
45. Silva EGD, Eulálio MDC, Souto RQ, Santos KDL, Melo RLPD, Lacerda AR. The capacity for resilience and social support in the urban elderly. Cienc Saude Coletiva [Internet]. 2019;24(1):7–16. doi:https://doi.org/10.1590/1413-81232018241.32722016. [Google Scholar] [PubMed] [CrossRef]
46. Covid C, Team R. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–March 16, 2020. Morb Mortal Wkly Rep [Internet]. 2020;69(12):343–6. [Google Scholar]
47. Bengtson VL, Silverstein M, Putney NM, Harris SC. Does religiousness increase with age? Age changes and generational differences over 35 years. J Sci Study Relig [Internet]. 2015;54(2):363–79. doi:https://doi.org/10.1111/jssr.12183. [Google Scholar] [CrossRef]
48. Bavel JJV, Baicker K, Boggio PS, Capraro V, Cichocka A, Cikara M, et al. Using social and behavioural science to support COVID-19 pandemic response. Nat Hum Behav [Internet]. 2020;4(5):460–71. doi:https://doi.org/10.1038/s41562-020-0884-z. [Google Scholar] [PubMed] [CrossRef]
49. Hoge R. A validated intrinsic religious motivation scale. J Sci Study Relig [Internet]. 1972;11(4):369–76. doi:https://doi.org/10.2307/1384677. [Google Scholar] [CrossRef]
50. Lwanga SK, Lemeshow S, Organization WH. Sample size determination in health studies: a practical manual [Internet]. England: World Health Organization; 1991. [Google Scholar]
51. Thai PQ, Rabaa MA, Luong DH, Tan DQ, Quang TD, Quach H-L, et al. The first 100 days of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) control in Vietnam. Clin Infect Dis [Internet]. 2021;72(9):e334–42. doi:https://doi.org/10.1093/cid/ciaa1130. [Google Scholar] [PubMed] [CrossRef]
52. Dillman DA. Mail and internet surveys: the tailored design method--2007 Update with new internet, visual, and mixed-mode guide [Internet]. New Jersey: John Wiley & Sons; 2011. [Google Scholar]
53. Joseph F, Barry JB, Rolph EA, Rolph EA. Multivariate data analysis [Internet]. New Jersey: Pearson Prentice Hall; 2010. [Google Scholar]
54. Ahorsu DK, Lin CY, Imani V, Saffari M, Griffiths MD, Pakpour AH. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addict [Internet]. 2022;2020(3):1–9. doi:https://doi.org/10.1007/s11469-020-00270-8. [Google Scholar] [PubMed] [CrossRef]
55. Nguyen HT, Do BN, Pham KM, Kim GB, Dam HT, Nguyen TT, et al. Fear of COVID-19 scale—associations of its scores with health literacy and health-related behaviors among medical students. Int J Environ Res Public Health [Internet]. 2020;17(11):4164. doi:https://doi.org/10.3390/ijerph17114164. [Google Scholar] [PubMed] [CrossRef]
56. Keyes CL, Wissing M, Potgieter JP, Temane M, Kruger A, van Rooy S. Evaluation of the mental health continuum-short form (MHC-SF) in setswana-speaking South Africans. Clin Psychol Psychother [Internet]. 2008;15(3):181–92. doi:https://doi.org/10.1002/(ISSN)1099-0879. [Google Scholar] [CrossRef]
57. Rogoza R, Truong Thi KH, Różycka-Tran J, Piotrowski J, Żemojtel-Piotrowska M. Psychometric properties of the MHC-SF: an integration of the existing measurement approaches. J Clin Psychol [Internet]. 2018;74(10):1742–58. doi:https://doi.org/10.1002/jclp.22626. [Google Scholar] [PubMed] [CrossRef]
58. Rigdon EE, Sarstedt M, Ringle CM. On comparing results from CB-SEM and PLS-SEM: five perspectives and five recommendations. J Res Manag [Internet]. 2017;39(3):4–16. doi:https://doi.org/10.15358/0344-1369-2017-3-4. [Google Scholar] [CrossRef]
59. Hair JF, Hult GTM, Ringle CM, Sarstedt M, Danks NP, Ray S. Evaluation of reflective measurement models. In: Partial least squares structural equation modeling (PLS-SEM) using R [Internet]. Cham: Springer; 2021. p. 75–90. [Google Scholar]
60. Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Mark Sci [Internet]. 2015;43(1):115–35. doi:https://doi.org/10.1007/s11747-014-0403-8. [Google Scholar] [CrossRef]
61. Hair JF, Hult GTM, Ringle CM, Sarstedt M, Richter NF, Hauff S. A primer on partial least squares structural equation modeling (PLS-SEM) [Internet]. Los Angeles: Sage; 2017. [Google Scholar]
62. Falk RF, Miller NB. A primer for soft modeling [Internet]. Ohio: University of Akron Press; 1992. [Google Scholar]
63. Hair JF, Sarstedt M, Hopkins L, Kuppelwieser VG. Partial least squares structural equation modeling (PLS-SEMan emerging tool in business research. Eur Bus Rev [Internet]. 2014;26(2):106–21. doi:https://doi.org/10.1108/EBR-10-2013-0128. [Google Scholar] [CrossRef]
64. Henseler J, Ringle CM, Sinkovics RR. The use of partial least squares path modeling in international marketing. In: New challenges to international marketing [Internet]. vol. 20. UK: Emerald Group Publishing Limited; 2009. p. 277–319. [Google Scholar]
65. Teerawichitchainan B, Pothisiri W, Long GT. How do living arrangements and intergenerational support matter for psychological health of elderly parents? Evidence from Myanmar, Vietnam, and Thailand. Soc Sci Med [Internet]. 2015;136(3):106–16. doi:https://doi.org/10.1016/j.socscimed.2015.05.019. [Google Scholar] [PubMed] [CrossRef]
66. Gausman J, Langer A. Sex and gender disparities in the COVID-19 pandemic. J Womens Health [Internet]. 2020;29(4):465–6. doi:https://doi.org/10.1089/jwh.2020.8472. [Google Scholar] [PubMed] [CrossRef]
67. Galasso V, Pons V, Profeta P, Becher M, Brouard S, Foucault M. Gender differences in COVID-19 attitudes and behavior: panel evidence from eight countries. Proc Natl Acad Sci [Internet]. 2020;117(44):27285–91. doi:https://doi.org/10.1073/pnas.2012520117. [Google Scholar] [PubMed] [CrossRef]
68. Długosz P. Factors influencing mental health among American youth in the time of the COVID-19 pandemic. Pers Indiv Differ [Internet]. 2021;175(428–450):110711. doi:https://doi.org/10.1016/j.paid.2021.110711. [Google Scholar] [PubMed] [CrossRef]
69. Kowalczyk O, Roszkowski K, Montane X, Pawliszak W, Tylkowski B, Bajek A. Religion and faith perception in a pandemic of COVID-19. Journal of Religion and Health [Internet]. 2020;59(6):2671–7. doi:https://doi.org/10.1007/s10943-020-01088-3. [Google Scholar] [PubMed] [CrossRef]
70. Vuong QH, Nguyen MH, Le TT. A mindsponge-based investigation into the psycho-religious mechanism behind suicide attacks [Internet]. Berlin: Walter de Gruyter GmbH; 2021. [Google Scholar]
71. Tung LT. Social responses for older people in COVID-19 pandemic: experience from Vietnam. J Gerontol Soc Work [Internet]. 2020;63(6–7):682–7. doi:https://doi.org/10.1080/01634372.2020.1773596. [Google Scholar] [PubMed] [CrossRef]
72. Vietnam UN. Un assessment of the social and economic impact of COVID-19 in Vietnam [Internet]. 2020. https://vietnam.un.org/en/95127-un-assessment-social-and-economic-impact-covid-19-viet-nam. [Google Scholar]
73. Westaway MS. The impact of chronic diseases on the health and well-being of South Africans in early and later old age. Arch Gerontol Geriatr [Internet]. 2010;50(2):213–21. doi:https://doi.org/10.1016/j.archger.2009.03.012. [Google Scholar] [PubMed] [CrossRef]
74. Lo Coco G, Gentile A, Bosnar K, Milovanović I, Bianco A, Drid P, et al. A cross-country examination on the fear of COVID-19 and the sense of loneliness during the first wave of COVID-19 outbreak. Int J. Environ Res Public Health [Internet]. 2021;18(5):2586. doi:https://doi.org/10.3390/ijerph18052586. [Google Scholar] [PubMed] [CrossRef]
75. Mahamid F, Bdier D, Berte D. Psychometric properties of the fear of COVID-19 scale (FCV-19S) in a Palestinian context. J Muslim Ment Health [Internet]. 2022;16(1):46–58. doi:https://doi.org/10.3998/jmmh.400. [Google Scholar] [CrossRef]
76. Overfield T. Biologic variation in health and illness: race, age, and sex differences [Internet]. Florida: CRC Press; 2017. [Google Scholar]
77. Koenig HG. Ways of protecting religious older adults from the consequences of COVID-19. Am J Geriatr Psychiatr [Internet]. 2020;28(7):776–9. doi:https://doi.org/10.1016/j.jagp.2020.04.004. [Google Scholar] [PubMed] [CrossRef]
78. Paterson J, Francis AJP. Influence of religiosity on self-reported response to psychological therapies. Ment Health Relig Cult [Internet]. 2017;20(5):428–48. doi:https://doi.org/10.1080/13674676.2017.1355898. [Google Scholar] [CrossRef]
79. James A, Wells A. Religion and mental health: towards a cognitive-behavioural framework. Br J Health Psychol [Internet]. 2003;8(3):359–76. doi:https://doi.org/10.1348/135910703322370905. [Google Scholar] [PubMed] [CrossRef]
80. Hayes SC, Strosahl KD, Bunting K, Twohig M, Wilson KG. What is acceptance and commitment therapy? A practical guide to acceptance and commitment therapy [Internet]. Berlin: Springer; 2004, p. 3–29. [Google Scholar]
81. Flaxman PE, Blackledge JT, Bond FW. Acceptance and commitment therapy: distinctive features [Internet]. New York: Routledge; 2010. [Google Scholar]
82. Shepherd K, Golijani-Moghaddam N, Dawson DL. ACTing towards better living during COVID-19: the effects of acceptance and commitment therapy for individuals affected by COVID-19. J Contextual Behav Sci [Internet]. 2022;23(27):98–108. doi:https://doi.org/10.1016/j.jcbs.2021.12.003. [Google Scholar] [PubMed] [CrossRef]
83. Yıldırım M, Güler A. COVID-19 severity, self-efficacy, knowledge, preventive behaviors, and mental health in Turkey. Death Stud [Internet]. 2022;46(4):979–86. doi:https://doi.org/10.1080/07481187.2020.1793434. [Google Scholar] [PubMed] [CrossRef]
84. Tran BX, Zhang MW, Le HT, Nguyen HD, Nguyen LH, Nguyen QLT, et al. What drives young Vietnamese to use mobile health innovations? Implications for health communication and behavioral interventions. JMIR mHealth and uHealth [Internet]. 2018;6(11):1–10. doi:https://doi.org/10.2196/mhealth.6490. [Google Scholar] [PubMed] [CrossRef]
85. Alam MZ, Alam MMD, Uddin MA, Mohd Noor NA. Do mobile health (mHealth) services ensure the quality of health life? An integrated approach from a developing country context. J Mark Commun [Internet]. 2022;28(2):152–82. doi:https://doi.org/10.1080/13527266.2020.1848900. [Google Scholar] [CrossRef]
86. van Dijk SDM, Bouman R, Folmer EH, den Held RC, Warringa JE, Marijnissen RM, et al. (Vi)-rushed into online group schema therapy based day-treatment for older adults by the COVID-19 outbreak in the Netherlands. Am J Geriatr Psychiatry [Internet]. 2020;28(9):983–8. doi:https://doi.org/10.1016/j.jagp.2020.05.028. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools