 Open Access
Open Access
ARTICLE
Examination of the Illness Representations among Children with T1DM in Relation to Mental Health Factors
1
Faculty of Medicine Department of Pediatrics, Pediatric Psychology and Psychosomatic Unit, Kálmán Laki Doctoral School,
University of Debrecen, Debrecen, 4032, Hungary
2
Department of Behavioural Sciences, University of Debrecen, Debrecen, 4032, Hungary
* Corresponding Author: Brigitta Munkácsi.
International Journal of Mental Health Promotion 2023, 25(8), 961-969. https://doi.org/10.32604/ijmhp.2023.027319
Issue published 06 July 2023
Abstract
The most common comorbid psychiatric disorders in children with type 1 diabetes mellitus (T1DM) are depression, anxiety and behavioral disorders. Patients with comorbid psychopathology are less capable of psychically adjusting to the new life situation resulting from T1DM, which may negatively affect glycemic control and adherence related to the treatment. We aimed to investigate the association between mental health and type 1 diabetes including illness representation. 115 children and adolescents with T1DM were recruited through the outpatient clinic in Debrecen, Hungary. Measures: PRISM-D, Child Depression Inventory (CDI), Cantril Ladder and Self-Rated Health, Glycosylaeted haemoglobin (HbA1C) were measured. Children having depressive symptoms drew fewer circles with less area. Children not drawing any important relationships possessed more depressive symptoms. Those diagnosed at a younger age displayed smaller distance between the Self- and Illness-circles. The PRISM-D test can be a promising tool to analyse emotional and cognitive representations and the psychological burden of T1DM.Graphic Abstract
Keywords
The most common comorbid psychiatric disorders in children with type 1 diabetes mellitus (T1DM) are depression, anxiety and behavioral disorders [1]. Patients with comorbid psychopathology are less capable of psychically adjusting to the new life situation resulting from T1DM [2], which may negatively affect glycemic control and adherence related to the treatment [3]. The improperly treated T1DM and the comorbid depression possibly lead to such negative medical consequences as a higher risk of hypoglycemic episodes [4,5], hospitalization for ketoacidosis [6] and lower health-related quality of life (HRQoL) [7].
Reynolds and Helgeson’s meta-analysis suggests that children with diabetes are at slightly elevated risk for psychological problems [8]. Based on the literature the relationship between childhood T1DM and depressive symptoms: adolescents with type 1 diabetes have more comorbid psychiatric conditions, for example depression. Those who have experience of sub-optimal glycemic control are more endangered for different types of comorbid psychiatric conditions, especially depression symptoms. Comorbid diabetes and depression symptoms may cause increased frequency of diabetes symptoms (e.g., DKA), elevated healthcare costs, more absences from school, decrease in self-management behaviors, and sub-optimal glycemic outcomes.
Since the results of case-control studies of depressive symptoms among T1DM-children are not congruent, a unitary conclusion cannot be drawn. The other most commonly measured dimension of mental health is satisfaction with life (SWL) which is a cognitive assessment of general quality of life-based on a person’s own criteria [9,10]. As the number of studies into discovering the association between T1DM and satisfaction with life is rather slight in terms of its significance, we have made it one of the main purposes of our research. Beside SWL, we have examined the self-rated health (SRH) of children with T1DM, which is an informative global indicator of health condition and quality of life [11–13]. Concerning studies conducted with adults, higher SRH scores predict better chances of survival [14,15]; better functional health condition [16]; as well as lesser extent of dependence on medical service [17]. According to Huang et al. [18] results, the female gender, the higher parental socioeconomic status (SES), the earlier disease onset, the shorter duration of T1DM as well as the lower HbA1c-level [19] contributed to higher self-rated health in children, adolescents and young adults. The SRH associated with the severity of the disease, the mental and social functions [20,21], and it is an important predictive factor of mortality and morbidity as well [22,23]. Self-rated health is one of the most significant global indicators of well-being and quality of life not only among adults as well as children, as it predicts to a higher accuracy the subsequent health condition and quality of life [24].
The examination of illness representations—the personal meaning of the disease [25]—can enrich with numerous important aspects the psychotherapy with children suffering from chronic disease. These representations determine what kind of implicit beliefs the patient develops about the disease and what kind of coping strategies the patient chooses [26,27].
On the basis of the results of international studies, the aim of our research was to examine the mental health of children with T1DM, with special consideration for satisfaction with life, self-rated health, frequency and severity of depressive symptoms as well as for the exploration of the association between these factors and the illness representations.
Our research questions were the followings:
1. How can be characterized the mental health status of children with T1DM, with special consideration for self-rated health and frequency and severity of depressive symptoms?
2. What kind of associations are there between the depression, satisfaction with life, future orientation and self-rated health?
3. What kind of associations are there between the mental health indicators and the illness representations?
4. What kind of associations are there between the diabetes-specific variables (e.g., T1DM duration, type of insulin therapy) and the illness representations?
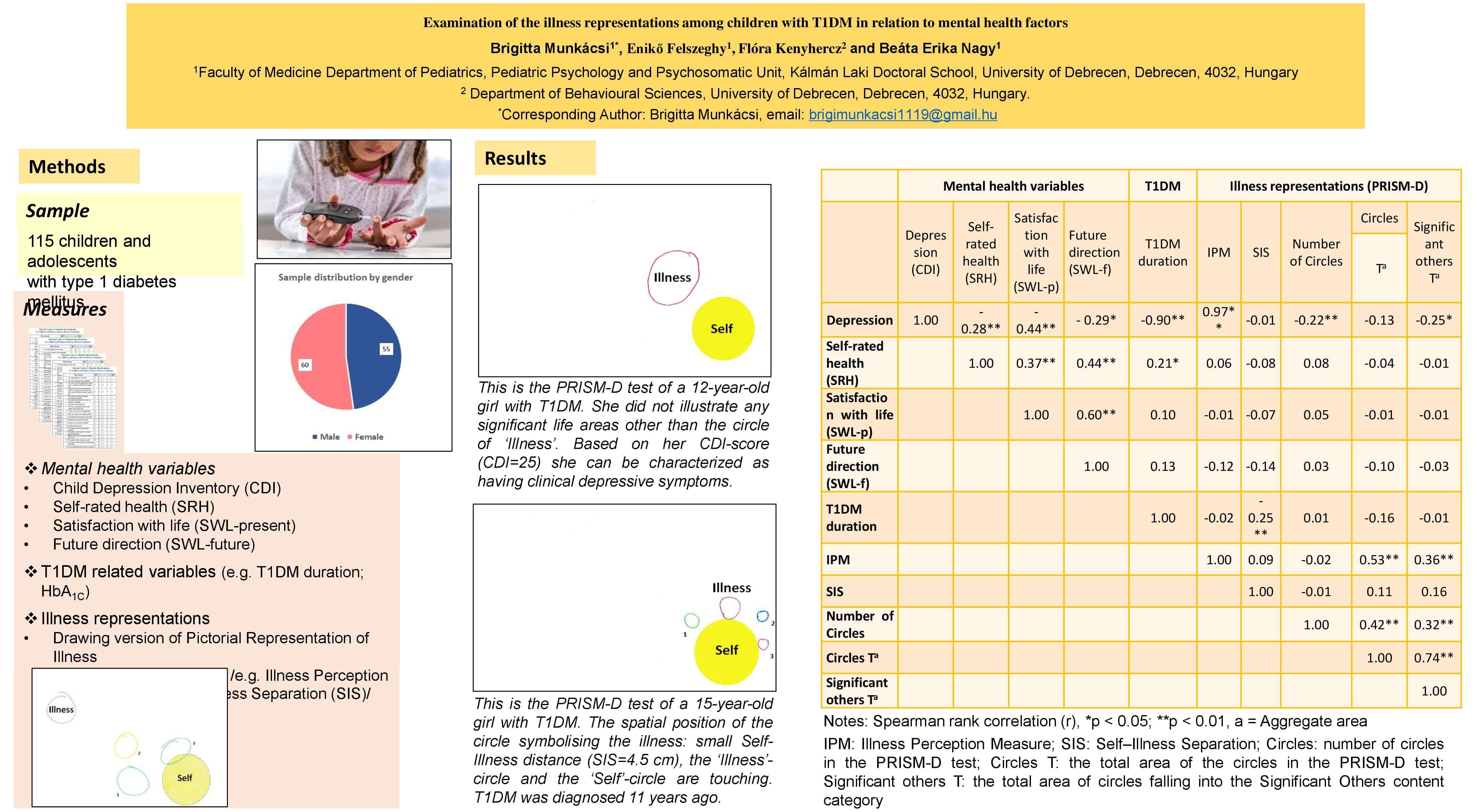
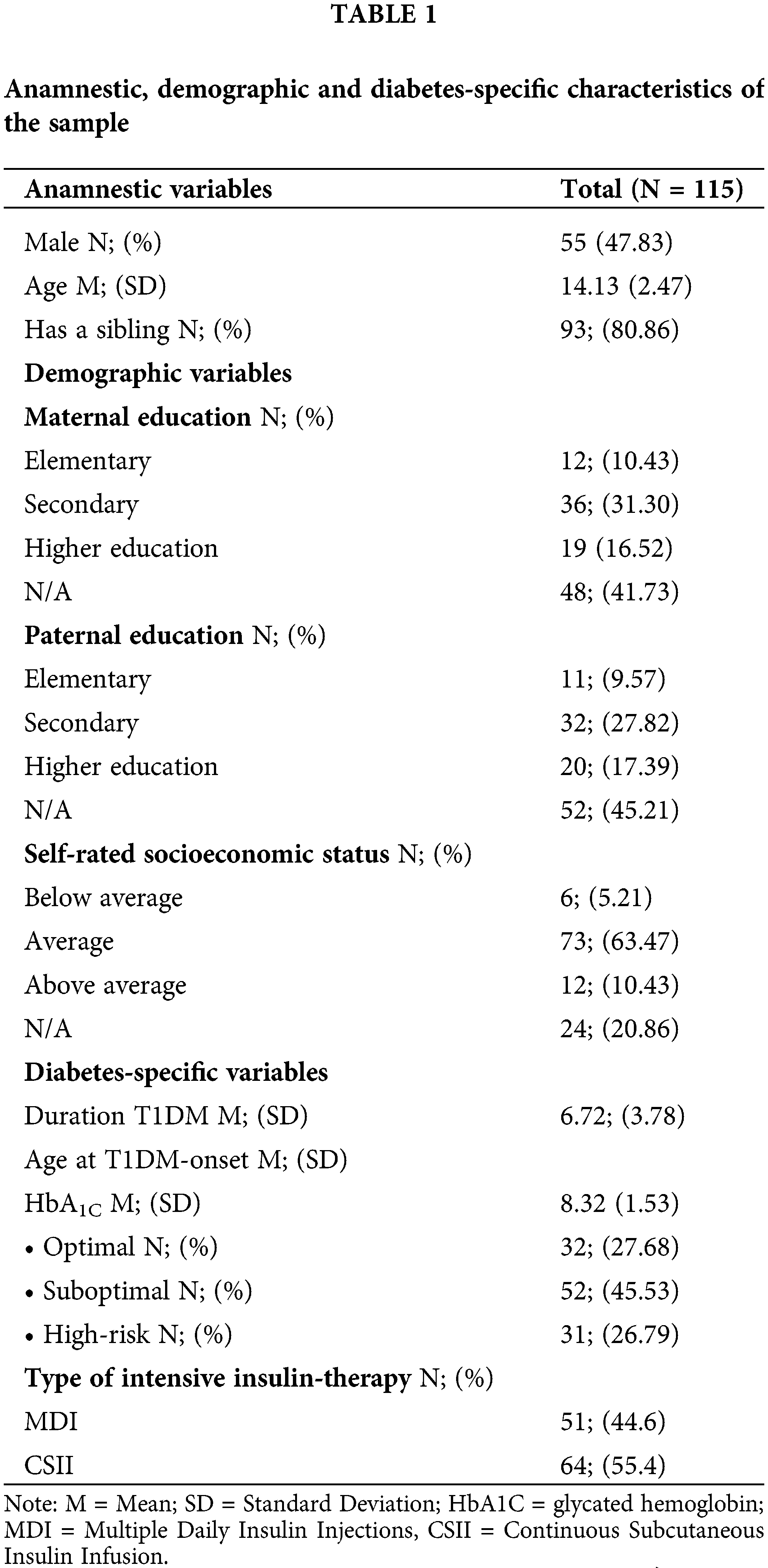
Our sample consisted of 115 T1DM children and adolescents. 60 girls (52.17%), 55 boys (47.83%) participated, and their mean age was 14.13, SD = 2.47 (min 8 – max 18). The mean duration of diabetes was 6.72, SD = 3.78 years. The mean value of HbA1C was 8.32 (SD = 1.53). 27.68% of the sample was of optimal HbA1C level, while 45.53% of sub-optimal, and 26.79% of high-risk HbA1C-level. Regarding the type of the applied intensive insulin therapy, we divided the children into two groups. 44.6% of the sample was treated with Multiple Daily Insulin Injections (MDI), while 55.4% was treated with insulin pump therapy (Continuous Subcutaneous Insulin Infusion, CSII) (Table 1). Data collection was carried out between September 2016 and December 2017 at the Endocrinology Outpatient Clinic Department of Pediatrics, University of Debrecen, Faculty of Medicine, Debrecen, Hungary.
Our sample includes all available observations from the Eastern region of Hungary. Our main inclusion criteria was the diagnosis of T1DM and the age of children (8–18). Our sample was assessed at the Pediatric Psychology and Psychosomatic Unit of the Department of Pediatrics of the University of Debrecen. The T1DM children participating in the research were being treated at the Endocrinology Unit of the Department of the Pediatrics of the University of Debrecen at the time of the study. The children and their parents were informed in writing before or after the endocrinology control examination about the possibility of participating in the research, its purpose, methods and voluntary nature. We asked the parents for written permission to conduct the study.
Our research was approved by the Regional Institutional Research Ethics Committee, Clinical Center, University of Debrecen (ID: 4528A-2016) following the ethical principles of the WMA Declaration of Helsinki. Written informed consent was obtained from all participants.
PRISM-D, drawing version of pictorial representation of illness self-measure [28,29]
The PRISM-D test is the drawing test version of PRISM test [28] developed by Hungarian researchers [29]. Participants have to present their disease on a white A/4 sheet by means of drawing a circle with a red marker. The white sheet symbolises the subject’s current life and the yellow pre-printed circle (7 cms in diameter) in the bottom-right corner represents the Self. First, according to the instruction, participants have to draw their disease on the test sheet without restriction as regards size and position [29]. Then, with optional colour markers, they may display significant factors that can currently be found in their lives. The distance between the centres of the Self-circle and the circle representing the disease (Self–Illness Separation, SIS) [28] implies the extent of the subjective distress caused by the disease. The size of the Illness-circle (Illness Perception Measure, IPM) [30] refers to the disease perception. This test can provide us with a picture of the complexity of the person’s life as well as the factors affecting recovery [31]. During data analysis, we analyzed SIS, IPM, the area and cumulated area, and the number of circles. We also categorised the circles on the basis of their primary meaning. The circles which the children had labelled were examined by three independent reviewers and rated into the following four main content categories: “Significant others”; “Free-time activities, hobbies”; “Future-related content, goals”; “School”. The framework created by Hungarian researchers served as the basis of categorization [29]. Since it is a system of categories developed on the adult sample, we have exchanged the category ‘Work’ with category ‘School’. We analyzed the frequency of content categories and the connection between illness representations and individual resources.
The cantril self-anchoring striving scale [32], life evaluation index [33]
We used the Life Evaluation Index [33] to measure SWL. The index was developed based on the 11 steps of the Cantril ladder [32]. The Cantril-ladder is a visual analogue scale, which means that the marked step indicates where the responders position themselves between the two endpoints of the scale. Children had to assess their satisfaction with life on an 11-step ladder both now and in five years. Step 10 of the ladder presents the highest, and step 0 presents the lowest level of satisfaction with life in both currently and in the future. The Cronbach-alpha is 0.91. Gallup [33] created the following three independent groups based on the points achieved on the scale:
1) ‘Thriving’: they are characterized by strong and consistent well-being. They view their current life situation as well as the next five years positively. They report significantly fewer health issues, less anxiety, stress, sadness and anger, and more happiness and enjoyment. In their case, the assessment as regards the present scores ≥7 points, and regarding the future ≥8 points.
2) ‘Struggling’: their well-being is inconsistent. They are moderately satisfied with their present and future life situations. Compared to the ‘Thriving’ group, they report a higher level of daily stress and anxiety and become ill twice as frequently.
3) ‘Suffering’: a high-risk group in respect of the development of mental disorders. They are slightly satisfied with their present life and their assessment for the next five years is rather low. They report more somatic symptoms, more severe disease burden, stress, anger, sadness. The assessment of the present and the future is ≤4 points.
Self-rated health, SRH [34]
We examined the self-rated health with the following question: ‘How would you assess your health compared to your peers?’, which children had to assess on a 4-point Likert-scale where 1 = ‘poor or bad’, 2 = ‘fair’, 3 = ‘good’, 4 = ‘excellent’. The question proved reliable both with adult and adolescent populations [34].
Child depression inventory, CDI [35–37]
CDI is a screening tool of 27 questions applied to measure the level of depression among children of 7 to 18 years of age, with three answer options (0,1,2) per question. Of the answers, ‘0’ stands for the absence of symptoms, ‘1’ for mild symptom manifestation, and ‘2’ for clinical level manifestation of symptoms for the previous two weeks. The maximum score is 54 points. The Cronbach-alpha is 0.92 [37].
The haemoglobin A1C (HbA1C) is an important diabetes-specific indicator. The HbA1c values for blood glucose control were collected from medical reports. The HbA1c test is the most commonly used measure of glycemic control and diagnostic test for T1DM (American Diabetes Association, 2003). We determined the severity of illness by the HbA1c indicator, which is recommended by the ISPAD. HbA1C <7.5 mmol represents optimal metabolic control, between 7.5–9.0 mmol suboptimal, while above 9.0 mmol means high-risk metabolic control [38].
We used IBM SPSS Statistics v22 for the statistical analysis of the data. The normality of the variables was assessed by Chi-square test and Kolmogorov-Smirnov test. As most of our variables did not display normal distribution, we used nonparametric statistical analysis. Descriptive statistics were used to analyse the variables of children’s mental health. We analyzed the associations between dependent and independent variables using Spearman rank correlation test, Kruskal-Wallis test and Mann Whitney U test.
Mental health factors of T1DM-children and adolescents
The mean CDI-score in the sample was 8.53 (SD = 5.96), in case of boys 7.2 (SD = 5.58), in case of girls 9.7 (SD = 6.09). We did not find significant gender difference (U = 958,00; p = 0.056), although the girls achieved a higher mean score. 75.5% of the T1DM-children belonged in the risk-free group. We found that 24.5% of the children showed subclinical depression while 11.76% of them were possible to characterize with clinical depression. Examining the association between the type of intensive insulin-therapy and depression, we found that 38.64% of the children treated with MDI showed subclinical depressive symptoms and 15.9% of them reported clinical depression. Among children receiving CSII therapy, only 17.24% reported subclinical symptoms, while 3.45% was characterized with clinical depression.
In our sample, the SRH mean of the T1DM-children was 2.74 (SD = 0.69). 60% of the children assessed their health good, 26.36% fair, 9.09% excellent, while 4.55% assessed it poor or bad. The mean SWL of the T1DM-children was 6.98 (SD = 1.89), and the mean of their future direction was higher, 8.13 (SD = 1.66). We did not find a significant difference between genders in terms of mental health factors and illness-specific variables.
Correlation between mental health variables
We found significant differences in mental health factors between groups created by the Life Evaluation Index [28]. Those who were classified into the “Thriving” group reported higher satisfaction with life regarding their present and future life condition as well. They achieved significantly lower CDI-scores (SWL-p: χ2 = 21.347; p < 0.01; SWL-f: χ2 = 6.977; p < 0.05) and better SRH (SWL-p: χ2 = 14.73; p < 0.01; SWL-f: χ2 = 18.949; p < 0.01) than the children in the groups “Struggling” and “Suffering”.
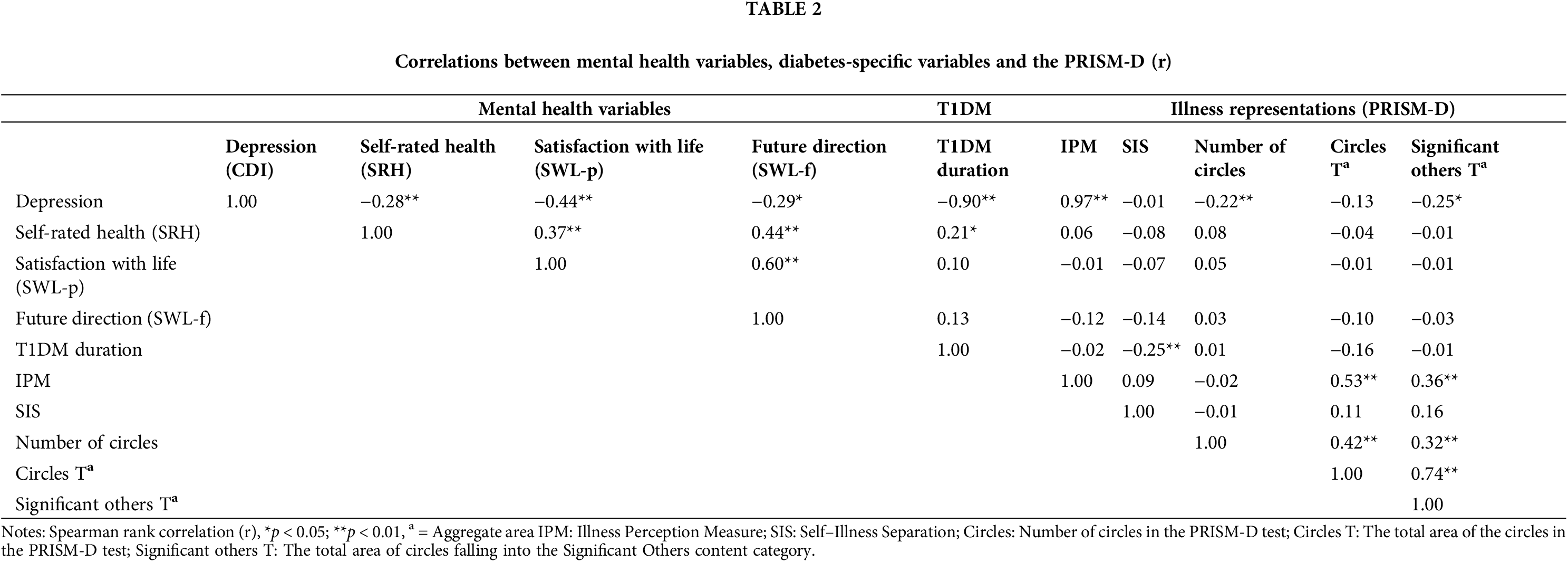
Examining the connection of the mental health variables, the strongest correlation was found between satisfaction with life and future direction. We found a moderate correlation between SRH and future direction as well as between satisfaction with life and future direction.
Association between T1DM-children and -adolescents’ mental health and illness representations
The most common content category was ‘Significant others’ (54.4%), followed by ‘Free-time activities’ (20.63%), then ‘Future-related content, goals’ (15.5%) and finally ‘School’ (6%). 14.16% of the children did not draw significant relationships, and 61% of them did not display any free-time activities, hobbies. 9.73% of the participants drew neither significant relationships nor any free-time activities, hobbies at the drawing test. Apart from the Illness-circle, 8.85% of them drew further content in connection with diabetes, and two children displayed only T1DM-related content. Those children, who did not draw significant relationships, reported a significantly higher depression score than those who drew at least one important personal relationship (U = 379.000; p = 0.01). Besides, they drew significantly fewer circles apart from the Illness-circle (U = 305.000; p < 0.01) furthermore the aggregate area of these circles was significantly smaller (U = 607.500; p < 0.05) (Figs. 1 and 2). We found a significant positive correlation between the sizes of the circles in the ‘Significant others’ category and the area of the Illness-circle (r = 0.360; p < 0.01), and between the number of the circles apart from the Illness-circle (r = 0.325; p < 0.01) and the aggregate area of theirs (r = 0.744; p < 0.01). Regarding the other content categories, no remarkable difference was identified concerning the factors of mental health.
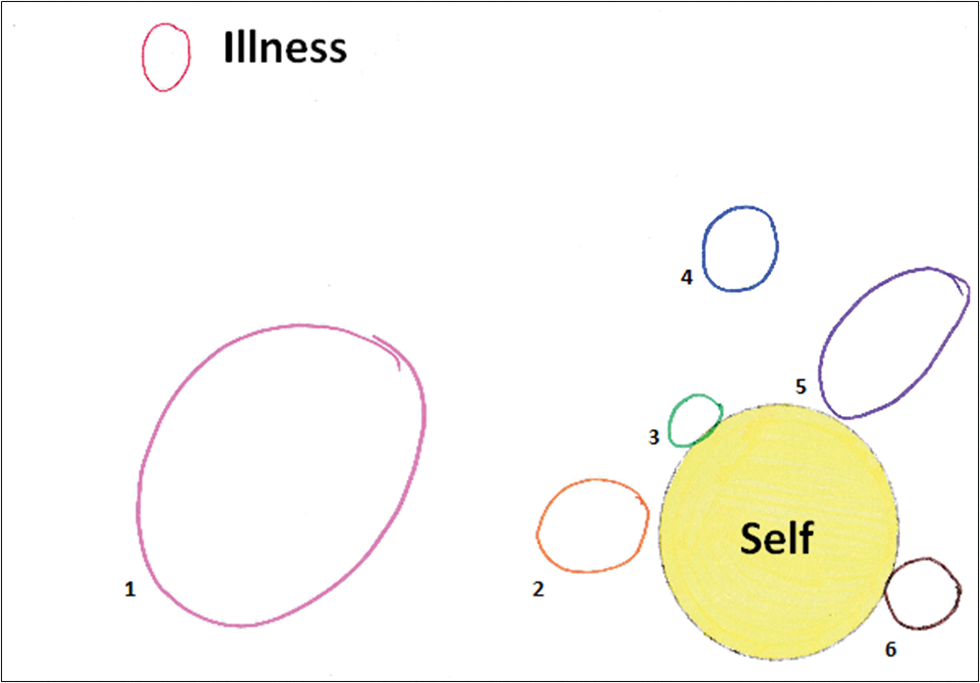
Figure 1: This is the PRISM-D test of a 9-year-old boy with T1DM. He illustrated 6 life areas that were important to him 3 of which could be classified into the content category ‘Significant others’ (‘Mom’, Jocóka’—sibling, ‘Cousins’). He did not report any depressive symptoms (CDI = 0).
Note: 1 = Environmental science class; 2 = Jocóka; 3 = Mom; 4 = Cousins; 5 = Maths competition; 6 = Maths study group.
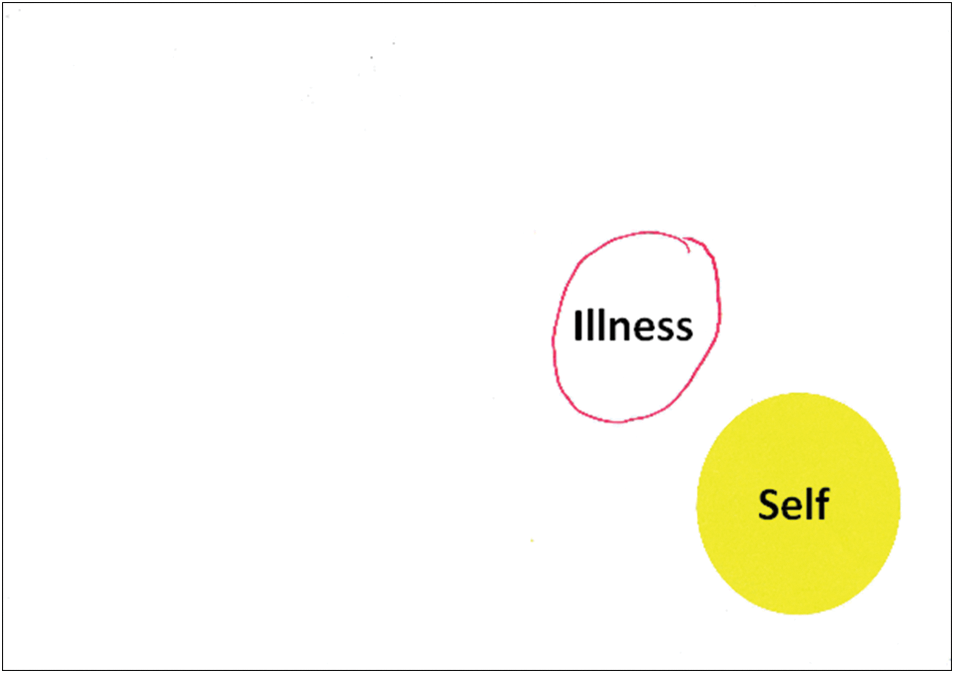
Figure 2: This is the PRISM-D test of a 12-year-old girl with T1DM. She did not illustrate any significant life areas other than the circle of ‘Illness’. Based on her CDI-score (CDI = 25) she can be characterized as having clinical depressive symptoms.
The mean SIS was 8.56 (SD = 4.0), and the mean IPM was 16.66 (SD = 28.41). Based on SIS, our sample can be characterized by a considerable degree of suffering from the disease. The lowest value was 0 cm, and the highest one was 23.5 cm.
Examining the connection between depression and the illness representations we found that the number of circles apart from the Illness-circle (r = −0.220; p < 0.05) and the sizes of the circles belonging in ‘Significant others’ (r = −0.253; p < 0.05) showed significant correlation with CDI-scores (Figs. 1 and 2). Besides, there appeared to be a tendentious association (r = −0.181; p = 0.069) between the number of the circles of ‘Significant others’ and CDI-scores. We did not find a significant difference between illness representations and the other factors of mental health (SRH, SWL-p, SWL-f).
The relation of diabetes-specific variables with mental health variables and illness representations
Examining the connection between the children’s illness representations and the duration of diabetes we found a significant negative correlation between the two variables, which means that the longer ago the diabetes was diagnosed, the lower the SIS-value was (r = −0.259; p < 0.01) (Figs. 3 and 4). Moreover, the duration of T1DM showed significant correlation with the SRH-index (r = 0.216; p < 0.05). Regarding the illness representations and the mental health factors, we did not find a significant connection with other diabetes-specific variables such as HbA1c, CSII or MDI (Table 2).

Figure 3: This is the PRISM-D test of a 15-year-old girl with T1DM. The spatial position of the circle symbolising the illness: small Self-Illness distance (SIS = 4.5 cm), the ‘Illness’-circle and the ‘Self’-circle are touching. T1DM was diagnosed 11 years ago.

Figure 4: This is the PRISM-D test of a 12-year-old boy with diabetes. The spatial position of the circle symbolising the illness: large Self-Illness distance (SIS = 21 cm). T1DM was diagnosed 6 years ago.
Note: 1 = Friends; 2 = Sport; 3 = Family.
Mental health factors of T1DM-children and adolescents
In studies applying the Child Depression Inventory, nearly a quarter of the examined T1DM-children: 22.8% [38], 23% [39], 25% [40] showed subclinical or clinical depressive symptoms. Similarly to the international results, this proportion in our research was 24.5%. However, according to McGrady et al. [41] results, the rate of clinical depression symptoms is 17.2% among T1DM-children. In this study, this proportion was merely 11.76%.
Previous studies using larger adult samples [42,43] identified as protective factors of SRH, the female gender, the shorter T1DM-duration, the younger age at the onset of disease, as well as the lower HbA1C-level. In the current study, however, we did not find such relations, which is likely explained by the small sample size and the diverse age-groups.
Comparing the T1DM-children’s satisfaction with life with the Hungarian results of HBSC [44], we can conclude that children living with diabetes are almost as satisfied with life as their healthy peers. We can conclude from our results that children with T1DM are satisfied with their lives to nearly the same extent as the children in the national representative sample. It means that the former ones do not consider T1DM as an inhibiting factor of their life, but as a condition highly possible to control through self-management.
Correlation of mental health variables
Children who were more satisfied with their present life and future direction fell by Gallup’s classification under the group ‘Thriving’. They are characterized by a particular stable, consistent well-being, and fewer health issues, negative feelings, stress and distress [45]. Our result, according to which the ‘Thriving’ reported significantly better health condition and fewer depressive symptoms, supports Gallup’s description. The lower level of self-rated health and a higher number of depressive symptoms (‘Struggling’ and ‘Suffering’) match the characteristics of these two groups as well. In many cases they have limited access to medical services and, as opposed to the group ‘Thriving’, they are characterized by twice as intense disease burden. The members of these two groups appear, therefore to be a high-risk group within the T1DM-population as regards the development of mental problems. For this reason, we consider it most important to screen this patient population for mental health issues within medical care.
Similarly to previous researches [46,47] examining the relationship between mental health variables, we found that those T1DM-children who reported better health condition, higher satisfaction with life and a more positive future direction were more likely to be characterized with significantly better emotional state.
The association between T1DM-children and adolescents’ mental health characteristics and their illness representations
During the analysis of PRISM-D test, we encountered with various meanings of content. Of the four categories that we established by content analysis, ‘Significant others’ appeared the most frequently. Based on our findings, we can conclude that the connection with family members and friends play an important role in the lives of T1DM-children. Those children who did not present meaningful personal relationships which could serve as resources to them through social support were far more likely to develop depressive symptoms. By using a nonverbal drawing test, we also confirmed the fact that the supportive social atmosphere in the child’s life is a highly crucial protective factor against the development of depression. The negative emotional state or mood the children reported manifested itself in the smaller number and size of the circles. T1DM-children with higher depression scores drew, on the one hand, significantly fewer circles (apart from the Illness-circle) and on the other hand the number and the size of the circles in the category ‘Significant others’ were considerably smaller. On the basis of the information mentioned above, we can conclude that the fewer resources there are in children’s lives, the less protected against the development of depressive mood they are.
In accord with the findings of Havancsák et al. [29], we found that the larger the ‘Illness’ and the ‘Significant others’ circles were, the larger they drew the circles symbolizing the resources too. One possible explanation for this can be the fact that the disease plays a more significant role in the patients’ lives, the more they need social support. The increase in the size of the circles can be explained with the possible mediating effect of distress. According to the results of previous studies, patients with higher anxiety drew significantly larger organs in projective drawing tests [48–50].
The associations between diabetes-specific variables, mental health variables and illness representations
Regarding diabetes-specific variables, mental health variables and illness representations we found that those children who were diagnosed earlier, drew the Illness-circle significantly closer to the Self-circle and reported higher levels of self-rated health than their more recently diagnosed counterparts. Our conclusion from this is that the experience of living diabetes as a chronic disease over the years—following the initial emotional shock reaction—can transform from a life-threatening state with compelling limitations into a sort of acceptive coexistence. The distance between the centre of the Self-circle and the centre of Illness-circle refers to the intensity of the subjective suffering [31]. Sándor et al. [31] found larger distance between the ‘Self’-circle and the ‘Illness’-circle (M = 10.62) among cancer patients. They explained this association with the highly intensive suffering from the disease. In the current study we found a somewhat smaller distance between the centres of the two circles (M = 8.56) in case of T1DM-children, however, not even on this basis may we consider their suffering from their illness marginal.
As limitations, we may mention that our results cannot be generalized for the population of T1DM children and interpretations are limited due to our non-representative small sample size. It would be undoubtedly beneficial to carry out into a broader cooperation a similar examination with a representative sample as well as a longitudinal study of the illness representations and mental health factors of the children population with diabetes. The repeatability of the test enables the clear monitoring of changes in the children’s representations and the improvement of their coping strategies. Additionally, due to the nature of self-reported questionnaires and measures, response biases (i.e., social desirability or recall bias) must be taken into consideration. Although there is no standard to compare our results to—since PRISM-D was originally established for the examination of adult illness representations and had never been used among children, but, at the same time, this is what makes our study a groundbreaking one.
The examination of illness representations adds important and new aspects of professional work with T1DM-children. Since the verbality-based and concrete conceptual thinking ability stabilizes after the age of 10, children can express their emotions, desires and fears by nonverbal tools such as drawings far more easily. We were the first to apply the PRISM drawing test to explore the illness representations of children—and among them of a special patients group: children with T1DM—and to examine the connection of these representations with various disease-specific variables and health indicators. With a more complex understanding of T1DM-children’s illness representations, their psychotherapic treatment can become more effective, which can positively affect their quality of life and their mental health which provided the novelty of the research.
When we investigate children with T1DM in a multiple way with quantitative and qualitative methods, deeper and more detailed results can be found. Also, applying PRISM-D test as a quantitative method we can see another side so the real self-esteem and mental representations of the children. This can support us not only in research findings but also in the individual psychological treatment of the patients. Based on our findings, we recommend the use of PRISM-D among T1DM-population as well as children living with other chronic diseases. The PRISM-D may be a feasible instrument to measure diabetes-related suffering. Furthermore, we can obtain a more complex understanding of children’s illness perception, emotional state and available resources, all of which can provide significant help in their individual and group psychotherapy.
Acknowledgement: The authors would like to thank all the children and parents for their participation. We are grateful to prof. György Balla and prof. Tamás Szabó, directors of the Department of Pediatrics for supporting our research, and our colleagues at the Pediatric Psychology and Psychosomatic Unit of the Department of Pediatrics of the University of Debrecen.
Funding Statement: The authors received no specific funding for this study.
Conflicts of Interest: The authors declare that they have no conflicts of interest to report regarding the present study.
Disclosure Statement of Preprints: Our work has been posted as a preprint on Research Square Platform through the In Review preprint service offered by SpringerNature.
Research Square, https://www.researchgate.net/publication/353094508_Examination_of_the_Illness_Representations_among_Children_with_T1DM_in_Relation_to_Mental_Health_Factors. doi:10.21203/rs.3.rs-494532/v1.
References
1. Kovács M, Obrosky DS, Goldston D, Drash A. Major depressive disorder in youths IDDM: a controlled prospective study of course and outcome. Diabetes Care [Internet]. 1997;20(1):45–51. doi:https://doi.org/10.2337/diacare.20.1.45. [Google Scholar] [PubMed] [CrossRef]
2. Lernmark B, Persson B, Fisher L, Rydelius PA. Symptoms of depression are important to psychological adaptation and metabolic control in children with diabetes mellitus. Diabet Med [Internet]. 1999;16(1):14–22. doi:https://doi.org/10.1046/j.1464-5491.1999.00008.x. [Google Scholar] [PubMed] [CrossRef]
3. Ducat L, Rubenstei A, Philipson LH, Anderson BJ. A review of the mental health issues of diabetes conference. Diabetes Care [Internet]. 2015;38(2):333–8. doi:https://doi.org/10.2337/dc14-1383. [Google Scholar] [PubMed] [CrossRef]
4. Rewers A, Chase HP, Mackenzie T, Walravens P, Roback M, Rewers M, et al. Predictors of acute complications in children with type 1 diabetes. JAMA [Internet]. 2002;287(19):2511–8. doi:https://doi.org/10.1001/jama.287.19.2511. [Google Scholar] [PubMed] [CrossRef]
5. Szabo S, Pibernik-Okanović M, Metelko Z. Quality of life assessment in the clinical care of diabetes and other chronic diseases: an overview of croatian experiences. Psychol Stud [Internet]. 2010;52(2):147–54. [Google Scholar]
6. Stewart SM, Rao U, Emslie GJ, Klein D, White PC. Depressive symptoms predict hospitalization for adolescents with type 1 diabetes mellitus. Pediatr [Internet]. 2005;115(5):1315–9. doi:https://doi.org/10.1542/peds.2004-1717. [Google Scholar] [PubMed] [CrossRef]
7. Grey M, Whittemore R, Tamborlane W. Depression in type 1 diabetes in children: natural history and correlates. J Psychosom Res [Internet]. 2002;53(4):907–11. doi:https://doi.org/10.1016/S0022-3999(02)00312-4. [Google Scholar] [PubMed] [CrossRef]
8. Reynolds KA, Helgeson VS. Children with diabetes compared to peers: depressed? Distressed? A meta-analytic review. Ann Behav Med [Internet]. 2011;42(1):29–41. doi:https://doi.org/10.1007/s12160-011-9262-4. [Google Scholar] [PubMed] [CrossRef]
9. Diener E. Subjective wellbeing: the science of happiness, and a proposal for a national index. Am Psychol [Internet]. 2000;55(1):34–43. doi:https://doi.org/10.1037/0003-066X.55.1.34. [Google Scholar] [CrossRef]
10. Frey MA, Ellis D, Templin T, Naar-King S, Gutai JP. Diabetes management and metabolic control in school-age children with type 1 diabetes. Child Health Care [Internet]. 2006;35(4):349–63. doi:https://doi.org/10.1207/s15326888chc3504_4. [Google Scholar] [CrossRef]
11. Kriston P, Pikó B, Kovács E. Self-rated health indicator as an indicator of mental well-being: behavioral epidemiological analysis of adolescent population. Orv Hetil [Internet]. 2012;153(47):1875–82. doi:https://doi.org/10.1556/OH.2012.29491. [Google Scholar] [PubMed] [CrossRef]
12. Compton WC. Toward a tripartite factor structure of mental health: subjective well-being, personal growth, and religiosity. J Psychol [Internet]. 2010;135(5):486–500. doi:https://doi.org/10.1080/00223980109603714. [Google Scholar] [PubMed] [CrossRef]
13. Jylha M, Guralnik JM, Ferrucci L, Jokela J, Heikkinen E. Is self-rated health comparable across cultures and genders? J Gerontol B Psychol Sci Soc Sci J [Internet]. 1998;53(3):144–52. [Google Scholar]
14. Han B, Phillips C, Ferrucci L, Bandeen-Roche K, Jylha M, Kasper J, et al. Change in self-rated health and mortality among community-dwelling disabled older women. Gerontol [Internet]. 2005;45(2):216–21. doi:https://doi.org/10.1093/geront/45.2.216. [Google Scholar] [PubMed] [CrossRef]
15. Ishizaki T, Kai I, Imanaka Y. Self-rated health and social role as predictors for 6-year total mortality among a non-disabled older Japanese population. Arch Gerontol Geriatr [Internet]. 2006;42(1):91–9. doi:https://doi.org/10.1016/j.archger.2005.05.002. [Google Scholar] [PubMed] [CrossRef]
16. Hillen T, Davies S, Rudd AG, Kieselbach T, Wolfe CD. Self-ratings of health predict functional outcome and recurrence free survival after stroke. J Epidemiology Community Health [Internet]. 2003;57(12):960–6. doi:https://doi.org/10.1136/jech.57.12.960. [Google Scholar] [PubMed] [CrossRef]
17. Long MJ, Marshall BS. The relationship between self-assessed health status, mortality, service use, and cost in a managed care setting. Health Serv Manag Rev [Internet]. 1999;24(4):20–7. [Google Scholar]
18. Huang GH, Palta M, Allen C, LeCaire T, D’Alessio D. Self-rated health among young people with type 1 diabetes in relation to risk factors in a longitudinal study. Am J Epidemio [Internet]. 2004;159(4):364–72. doi:https://doi.org/10.1093/aje/kwh055. [Google Scholar] [PubMed] [CrossRef]
19. Undén AL, Elofsson S, Andréasson A, Hillered E, Eriksson I, Brismar K. Gender differences in self-rated health, quality of life, quality of care, and metabolic control in patients with diabetes. Gender Medicine [Internet]. 2008;5(2):162–80. doi:https://doi.org/10.1016/j.genm.2008.05.003. [Google Scholar] [PubMed] [CrossRef]
20. Shibuya K, Hashimoto H, Yano E. Individual income, income distribution, and self- rated health in Japan: cross sectional analysis of nationally representative sample. BMJ [Internet]. 2002;5324(7328):16–9. doi:https://doi.org/10.1136/bmj.324.7328.16. [Google Scholar] [PubMed] [CrossRef]
21. Garratt AM, Schmidt L, Fitzpatrick R. Patient-assessed health outcome measures for diabetes: a structured review. Diabet Med [Internet]. 2002;19(1):1–11. doi:https://doi.org/10.1046/j.1464-5491.2002.00650.x. [Google Scholar] [PubMed] [CrossRef]
22. Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav [Internet]. 1997;38(1):21–37. doi:https://doi.org/10.2307/2955359. [Google Scholar] [CrossRef]
23. Bond J, Dickinson HO, Matthews F, Jagger C, Brayne C. Self-rated health status as a predictor of death, functional and cognitive impairment: a longitudinal cohort study. Eur J Ageing [Internet]. 2006;83(4):193–206. doi:https://doi.org/10.1007/s10433-006-0039-8. [Google Scholar] [PubMed] [CrossRef]
24. Viner RM, Ozer EM, Denny S, Marmot M, Resnick M, Fatusi A, et al. Adolescence and the social determinants of health. Lancet [Internet]. 2012;379(9826):1641–52. doi:https://doi.org/10.1016/S0140-6736(12)60149-4. [Google Scholar] [PubMed] [CrossRef]
25. Széll K, Kiss E. Investigation of the relationship between disease representation and quality of life in people with stomach. In: Kiss E, Polyák L, editors. Health rehabilitation booklets II. The role of personal and social factors in rehabilitation work [Internet]. Budapest: Oriold and Partners Publisher; 2012. [Google Scholar]
26. Kuzucu Y, Şimşek ÖF, Koşe-Demiray Ç. Language and the symptoms of mental illness connection via abstract representations of the self and the world. J Psychol [Internet]. 2020;154(3):214–32. doi:https://doi.org/10.1080/00223980.2019.1703098. [Google Scholar] [PubMed] [CrossRef]
27. Petrie KJ, Weinman J. Patients’ perceptions of their illness: the dynamo of volition in health care. Curr Dir Psychol Sci [Internet]. 2012;20(10):1–6. doi:https://doi.org/10.1177/0963721411429456. [Google Scholar] [CrossRef]
28. Büchi S, Sensky T. PRISM: pictorial representation of illness and self measure: a brief nonverbal measure of illness impact and therapeutic aid in psychosomatic medicine. Psychosomatics [Internet]. 1999;40(4):314–20. doi:https://doi.org/10.1016/S0033-3182(99)71225-9. [Google Scholar] [PubMed] [CrossRef]
29. Havancsák R, Pócza-Véger P, Csabai M. The PRISM-D drawing test in the study and treatment of hospital patients. In: Csabai M, Pintér JN, (eds.) Psychology in Healing. Phenomenological, Art Psychological and Body-Centered Approaches. Oriold and Partners Publisher; 2013. p. 83–107. [Google Scholar]
30. Reimus JL, Vingerhoets AJ, Soons PH, Korstanje MJ. Suffering in psoriasis patients: its relation with illness severity and subjective well-being. Int J Dermatol [Internet]. 2007;46(10):1042–5. doi:https://doi.org/10.1111/j.1365-4632.2007.03191.x. [Google Scholar] [PubMed] [CrossRef]
31. Sándor Z, Csabai M. Using the PRISM-D drawing test to complex examination of emotional and cognitive representations related to cancer disease. Orv Hetil [Internet]. 2018;159(48):2021–30. doi:https://doi.org/10.1556/650.2018.31181. [Google Scholar] [PubMed] [CrossRef]
32. Cantril H. The pattern of human concern [Internet]. Rutgers University Press; 1965. [Google Scholar]
33. Gallup DS. Worldwide research methodology and codebook. Gallup Inc.; 2016. [Google Scholar]
34. Pikó B, Barabás K, Boda K. The epidemiology of psychosomatic symptoms and their effect on self-esteem in health among university students. Orv Hetil [Internet]. 1995;136(31):1667–71. [Google Scholar] [PubMed]
35. Kovacs M. Children’s depression inventory (CDI). Multi-Health Systems Inc.; 1992. [Google Scholar]
36. Kovacs M. The children’s depression inventory (CDI). Psychopharmacol Bull [Internet]. 1985;21(4):995–8. [Google Scholar] [PubMed]
37. Rózsa S, Vetró Á, Komlósi VA, Gádoros J, Kő N, Csorba J. Questionnaire measurement of depression in children and adolescents based on clinical and normative sample experience. Psychopharmacol Bull [Internet]. 1999;19(4):459–82. [Google Scholar]
38. de Wit M, Gajewska KA, Goethals ER, McDarby V, Zhao XL, Hapunda G, et al. ISPAD clinical practice consensus guidelines 2022: psychological care of children, adolescents and young adults with diabetes. Pediatr Diabetes [Internet]. 2022;23(8):1373–89. doi:https://doi.org/10.1111/pedi.13428. [Google Scholar] [PubMed] [CrossRef]
39. Hood KK, Rausch JR, Dolan LM. Depressive symptoms predict change in glycemic control in adolescents with type 1 diabetes: rates, magnitude, and moderators of change. Diabetes Care [Internet]. 2011;12:718–23. [Google Scholar]
40. Goad K. Examining the mental health issues prevalent in adolescent type-1 diabetics: an evidence-based review to improve health. J Diabetes Metab [Internet]. 2015;6(9):599. [Google Scholar]
41. McGrady ME, Hood KK. Depressive symptoms in adolescents with type 1 diabetes: associations with longitudinal outcomes. Diabetes Res Clin Pract [Internet]. 2010;88(3):35–7. doi:https://doi.org/10.1016/j.diabres.2010.03.025. [Google Scholar] [PubMed] [CrossRef]
42. Németh Á, Költő A. Health behaviour in school-aged children (HBSCWHO-collaborative cross-national study national report. NEFI; 2014. [Google Scholar]
43. Huang GH, Palta M, Allen C, LeCaire T, D’Alessio D. Self-rated health among young people with type 1 diabetes in relation to risk factors in a longitudinal study. Am J Epidemiol [Internet]. 2004;159(4):364–72. doi:https://doi.org/10.1093/aje/kwh055. [Google Scholar] [PubMed] [CrossRef]
44. de Wit M, Snoek FJ. Depressive symptoms and unmet psychological needs of Dutch youth with type 1 diabetes: results of a web-survey. Pediatr Diabetes [Internet]. 2011;12(3):172–6. doi:https://doi.org/10.1111/j.1399-5448.2010.00673.x. [Google Scholar] [PubMed] [CrossRef]
45. Undén AL, Elofsson S, Andréasson A, Hillered E, Eriksson I, Brismar K. Gender differences in self-rated health, quality of life, quality of care, and metabolic control in patients with diabetes. Gend Med [Internet]. 2008;5(2):162–80. doi:https://doi.org/10.1016/j.genm.2008.05.003. [Google Scholar] [PubMed] [CrossRef]
46. Gallup DS. Worldwide research methodology and codebook [Internet]. Gallup Inc.; 2016. [Google Scholar]
47. Pikó B. Self-perceived health among adolescents: the role of gender and psychosocial factors. Eur J Pediatr [Internet]. 2007;166(7):701–8. doi:https://doi.org/10.1007/s00431-006-0311-0. [Google Scholar] [PubMed] [CrossRef]
48. Swami V, Chamorro-Premuzic T, Sinniah D, Maniam T, Kannan K, Stanistreet D, et al. General health mediates the relationship between loneliness, life satisfaction and depression. Soc Psychiatry Psychiatr Epidemiol [Internet]. 2007;42(2):161–6. doi:https://doi.org/10.1007/s00127-006-0140-5. [Google Scholar] [PubMed] [CrossRef]
49. Broadbent E, Petrie KJ, Ellis CJ, Ying J, Gamble G. A picture of health–myocardial infarction patients’ drawings of their hearts and subsequent disability: a longitudinal study. J Psychosom Res [Internet]. 2004;57(6):583–7. doi:https://doi.org/10.1016/j.jpsychores.2004.03.014. [Google Scholar] [PubMed] [CrossRef]
50. Látos M, Barabás K, Lázár G, Szederkényi E, Szenohradszky P, Marofka F. Mental representations of the new organ and posttransplant patients’ anxiety as related to kidney function. Transplant Proc [Internet]. 2012;44(7):2143–6. doi:https://doi.org/10.1016/j.transproceed.2012.07.097. [Google Scholar] [PubMed] [CrossRef]
Cite This Article
 Copyright © 2023 The Author(s). Published by Tech Science Press.
Copyright © 2023 The Author(s). Published by Tech Science Press.This work is licensed under a Creative Commons Attribution 4.0 International License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.


 Submit a Paper
Submit a Paper Propose a Special lssue
Propose a Special lssue View Full Text
View Full Text Download PDF
Download PDF Downloads
Downloads
 Citation Tools
Citation Tools