Melatonin Ameliorates Hippocampal Excitotoxicity and Neuroinflammation in Permanent MCAO by Targeting NMDA/AMPA Receptors and the NLRP3 Inflammasome via Nrf2/PPARγ/JNK/NF-κB Crosstalk
Abdullah Alattar1, Reem Alshaman1, Fawaz E. Alanazi1, Yusuf S. Althobaiti2, Ghareb M. Soliman3, Waleed Salman Khubrni1, Howaida S. Ali4, Fawad Ali Shah5,6,*
1 Department of Pharmacology and Toxicology, Faculty of Pharmacy, University of Tabuk, Tabuk, 71491, Saudi Arabia
2 Department of Pharmacology and Toxicology, College of Pharmacy, Addiction and Neuroscience Taif University, Taif, 21944, Saudi Arabia
3 Department of Pharmaceutics, Faculty of Pharmacy, University of Tabuk, Tabuk, 71491, Saudi Arabia
4 Department of Pharmacology, Faculty of Medicine, University of Tabuk, Tabuk, 71491, Saudi Arabia
5 Swat College of Pharmaceutical Sciences (SCPS), Gogdara, Swat, 19200, Khyber Pakhtunkhwa, Pakistan
6 Riphah Institute of Pharmaceutical Sciences, Riphah International University, Islamabad, 44000, Pakistan
* Corresponding Author: Fawad Ali Shah. Email: 
(This article belongs to the Special Issue: Neuroinflammation and Neuroprotection in CNS Diseases: From Mechanisms to Therapeutic Targets)
BIOCELL https://doi.org/10.32604/biocell.2026.074865
Received 20 October 2025; Accepted 04 January 2026; Published online 22 January 2026
Abstract
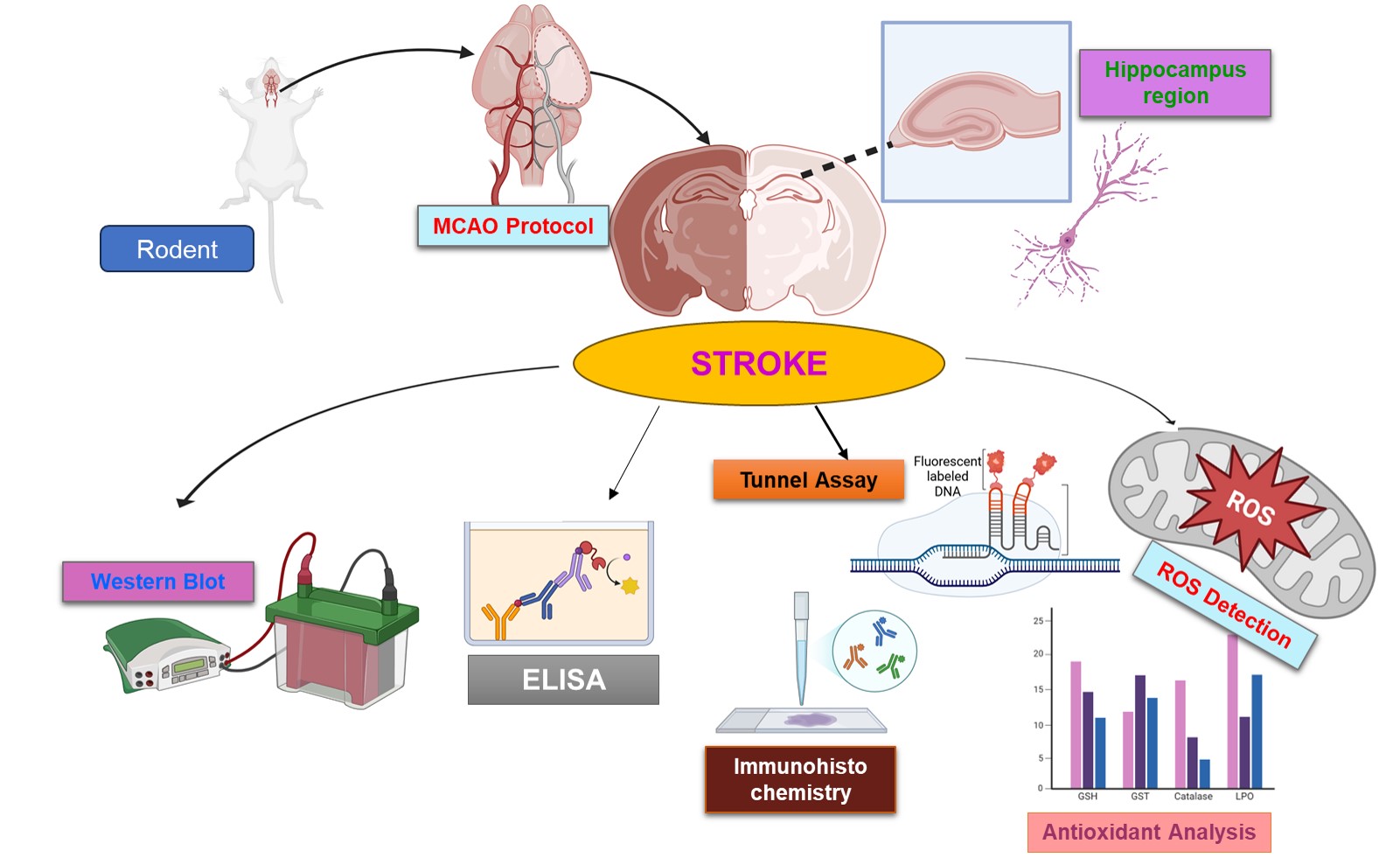
Objectives: Permanent middle cerebral artery occlusion (pMCAO) can lead to hippocampal damage through multiple linked pathways such as reactive oxidative stress (ROS), neuroinflammation mediated by NOD-, LRR- and pyrin domain-containing protein 3 (NLRP3), tumour necrosis factor-alpha (TNF-α), and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), and glutamate excitotoxicity involving N-methyl-D-aspartate receptor subunits 2a and 2b (NR2a/NR2b) and α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (AMPAR/GluR1). The hippocampus, which is essential for memory and cognition, is at a substantial risk of ischemic degeneration. The aim of this study was to investigate the neuroprotective potential of melatonin in regulating these pathways.
Method: Male adult rats were subjected to pMCAO, and melatonin (5 mg/kg) was administered just prior to ischemia, while sham-operated animals underwent surgery without nylon insertion. Hippocampal samples were collected 24 h after ischemia,
Results: Hippocampal tissues showed NLRP3 inflammasome activation, increased TNF-α and p-NF-κB, and decreased peroxisome proliferator-activated receptor (PPARγ) after pMCAO. Melatonin-modulated ischemia-induced glutamatergic receptor subunits (NR2a, NR2b, GluR1) dysregulation, which possibly stimulated the prosurvival pathways and reduced collagen response-mediated protein (CRMP2) and its phosphorylation. Melatonin also modulated the expression of the postsynaptic protein (PSD95) and inhibited inflammatory cascades while upregulating antioxidant proteins. Further, melatonin reduced inflammation triggered by NLRP3, restored synaptic integrity, possibly by enhancing nuclear factor erythroid 2-related factor 2 (Nrf2) expression.
Conclusion: These results demonstrated the dual role of melatonin by protecting ischemic brain damage both as a modulator of excitotoxicity and neuroinflammation/oxidative stress.
Graphical Abstract
Keywords
Ischemic stroke; melatonin; hippocampus; glutamatergic receptor
 Open Access
Open Access